As much as I didn't want to we had too. Our monthly infusion was due. Wednesday we were scheduled to check into clinic at 10am, then on to physical therapy before we hit the pool. Unfortunately, as we pulled into the hospital Gary had an accident in his pants. There went the pool. It honestly instantly upset me because I thought it was over. He had gone for 24 hours without going potty so I thought for sure the next time it would be over which would have confirmed a virus.
When we went up to clinic, I was close to tears. I didn't want to run Remicade. I didn't want this to be an issue. The nurse asked me about meds. I looked at her and said, "I am having a moment. I need a minute. I am so frustrated. I am not frustrated which anyone here. I am frustrated with the situation. I thought for sure this was a bug." I went on and on. She was very comforting. In past months, she had not said much to me which I found strange. I wasn't offended by the way she was stand offish. People have their reasons. I am realize not everything is about me. So I just went with it. She was polite enough so. Suddenly, in the rawness of our emotions, she let it go. She had recently had a baby. I heard about but wasn't given details so decided to mind my business. As tears filled my eyes she let me know her newborn went 17 minutes without oxygen at birth. She said despite what tests say she does not seem to have the brain damage she says she does. Her baby is making the progress she is suppose too. They take each day one at a time.
I thanked her for sharing her personal experience with me. I told her it meant a lot. We laughed as I asked her not to tell them I was crying.
When our doctors came in we talked about a plan of attack. She gave me a couple different options. We could run the Cytoxan, IVIG, Methopred, and Pamidronate as planned. Then the next week another pulse with Remicade for what we thought was the return of his IBD. Second was to run the Remicade, methopred, pamidronate and wait on the IVIG. Push the IVIG and steroid pulse to the next week. I wanted to go with the first option. I wanted to give his bowels more time. This potentially still could be a bug. But what I didn't like is this virus is making his JDM go bonkers. Labs are fine but that matters not.
The hospital stay was the worst. Well, I cant think of others stays that matched but, shared room, very small, next to the nurses station. Our roommate had to dominate the bathroom because he was there for colon issues as well. Fortunately, Gary didn't not have to use the bathroom. In twenty four hours plus, we did not once enter the bathroom in our room. Gary used the urinal. I had to walk down the hall. I could list all the mistakes and details. All around, it truly was terrible. It was even more terrible when the doctor came in that evening to suggest maybe the return of Gary's diarrhea was from milk or from gluten. I was close to ripping out his IV and walking out of there. It is the style I am not use to but just the same it was the last thing I wanted to hear. Are you telling me we gave him Remicade because of simple intolerances? Why wasn't that explored before running three months of treatment. By the way that same treatment cured his diarrhea within 24 hours of running. How is that an intolerance. I was ready to run. I am not against it. It very well could be. But a biospy and blood panel said there was no evidence of that. The night was long. Gary was miserable. Although the IV start went very well, the infusions themselves were hard. I am strongly leaning towards having a port put in. His veins seems to be burnt or stripped or something. He acts like he is being infused with acid. I'm just so done with it. I know that doctors will be upset with me. I know my family will too. But I have to do what is right for him. He can't do this anymore.
Thank you Summer!
Welcome to Gary's Mission to Remission! Juvenile Dermatomyositis, a rare autoimmune disease.
Monday, May 28, 2012
Tuesday, May 22, 2012
Don't Want To Go Back
Instead of the gagging being a side effect of methotrexate, it actually wasn't it. It was a start of a storm. A stomach flu storm. Wednesday night he had the return of the evil diarrhea. Thursday, tummy pain. More diarrhea then vomiting. He continued to run around so it was confusing. Friday morning, vomiting and diarrhea, from both ends. Oddly enough he was not "ill" but was getting run down. Friday night, with my high heals on, all dressed up for a birthday party I was suppose to go to for a good friend, I spent snuggle him, worried. Mom slipped back into her pajama's, and back to bed we went. Gary slept a long time.
All of his calcium deposits were enlarged. No fever, but he began to throw up the water he drank and continued with diarrhea. Saturday morning I had enough. We called the rheumatology doc on call at Seattle Children's, packed him up, and headed in. I didn't feel like I could keep in front of his hydration. He was red with a rash that looked like he had scratched up a storm which he had not. This bug denoted on Wednesday evening because that is when the rash appeared. Much like the one he had at diagnosis. His JDM looked like it was glowing bright.
Once in the emergency room, labs were taken. They gave me a choice to take him home if I felt confident I could keep him hydrated. I didn't feel that way. His food aversion and now drink aversion was troublesome. Hydration through IV was the best bet in my book. They agreed and admitted us. That night he put a special show on in the bathroom. Never seen something like that. I mean, on the walls even. Explosive to say the least. Every time he nibbled on food it was consequence. We waited till Sunday night to leave just to make sure.
We discovered he has open sores on the insides of his cheeks and on the roof of his mouth. They don't seem to bother him with pain. The more I get a peak of it I think it might be thrush. He is on medication to treat that so not sure why it is not working.
I am so glad he is doing so much better. We weren't sure exactly what he had but now everything seems to be subsiding, everything is coming back on line, it looks for sure it was a gasteronitis bug of some kind. I do think it is doing nothing for his JDM but it is a wait and see. His labs were fine. His C. reactive protein was elevated again but the virus can cause that. Right. Sure it can.
Today he was well enough to go get his eye's checked. Checked out A okay. Then we went onto PT. On the way there I gave him his vitamin D and calcium chocolate chew. He told me it tasted bad which he had never complained about before. He chewed it much longer than he has ever. It somehow turned it into a taffy, stringy like, texture which suddenly, he decided to gag and choke on while I drove down the road. It gagged him and once again, he brought up the entire contents of his tummy. All over the back of the car. I couldn't get him to talk to me so I began lane changing frantically planning a straight shot to the town's emergency room which was 6 blocks away. I yelled for him to talk. He couldn't because he was to busy heaving. I finally saw a gasp of air. Then another. Then another. Then the car smelled like a someone rode the merry go round to long. If I have to be around barf another second , I am gonna lose it.
Well not really. But I am growing tired of it. A little buck naked action in a parking lot at the grocery store to change clothes. Ran in bought paper towels and 409 cleaner to so some damage control in the back seat. It was interesting he had a hard time walking around, grapping at his legs periodically saying his legs hurt.
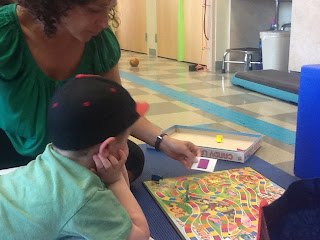
Later at physical therapy he definitely was crabby. He was not cooperating with any body that day. She tried stretching him out and said his range of motion seems good today but he is also tender to the touch he seems like. She made a comment to me that when he doesn't want to do a certain task, he says he is tired. If it is something he enjoys then he does it no problem. I wasn't sure how to take that. I mean, it is true. But don't we all? I already knew this about him. Gary's brother and sister are the same way. Something they don't enjoy, well, let the drama roll. He does not however, fake anything. I don't think she was implying that but unfortunately after a long weekend in the hospital, a long day, I must have been sensitive.
Tomorrow we have to go back. I really don't want too. I even contemplated asking for a reschedule for later in the week. I can only imagine how Gary feels about it. He needs to be followed though. He needs his treatments to make sure we are staying in front of the JDM or extinguishing fires from this nasty bug. Five days of not being right. One thing we have to look forward to tomorrow is before we go to the floor to start his IV and get meds going, we are meeting PT at the pool. She is going to do some work in the pool.
He is in good spirits, so I am grateful. Tired but grateful.
DAD GOING DOWN
Since it was the weekend, it was nice to have my husband with me finally. Well until the IV was started. My husband was holding his hand while Gary screamed, when his head went down. The nurse called over to him, "ARE YOU OK SIR". He was pale and spinning. We told him to sit. It distracted Gary for sure but we thought Dad was going to hit the floor. It took him about ten minutes for the color to return to his face. This is the first time a relative has had this reaction. My niece did the same thing. Oh boy.
WHAT MAKES ME SAD
The happy boy is gone. He was here when the antibiotics were in his system. So was his strength. His strange euphoric happiness we just couldn't get enough of. He was good hearted, loving, caring, amazingly happy. He is back to the ornery, inpatient, not on top of the world kid. I have even asked the doctors, why? Why is that? Why is this guy back? Not saying I want to run antibiotics but it just seems funny to me.
All of his calcium deposits were enlarged. No fever, but he began to throw up the water he drank and continued with diarrhea. Saturday morning I had enough. We called the rheumatology doc on call at Seattle Children's, packed him up, and headed in. I didn't feel like I could keep in front of his hydration. He was red with a rash that looked like he had scratched up a storm which he had not. This bug denoted on Wednesday evening because that is when the rash appeared. Much like the one he had at diagnosis. His JDM looked like it was glowing bright.
Once in the emergency room, labs were taken. They gave me a choice to take him home if I felt confident I could keep him hydrated. I didn't feel that way. His food aversion and now drink aversion was troublesome. Hydration through IV was the best bet in my book. They agreed and admitted us. That night he put a special show on in the bathroom. Never seen something like that. I mean, on the walls even. Explosive to say the least. Every time he nibbled on food it was consequence. We waited till Sunday night to leave just to make sure.
We discovered he has open sores on the insides of his cheeks and on the roof of his mouth. They don't seem to bother him with pain. The more I get a peak of it I think it might be thrush. He is on medication to treat that so not sure why it is not working.
I am so glad he is doing so much better. We weren't sure exactly what he had but now everything seems to be subsiding, everything is coming back on line, it looks for sure it was a gasteronitis bug of some kind. I do think it is doing nothing for his JDM but it is a wait and see. His labs were fine. His C. reactive protein was elevated again but the virus can cause that. Right. Sure it can.
Today he was well enough to go get his eye's checked. Checked out A okay. Then we went onto PT. On the way there I gave him his vitamin D and calcium chocolate chew. He told me it tasted bad which he had never complained about before. He chewed it much longer than he has ever. It somehow turned it into a taffy, stringy like, texture which suddenly, he decided to gag and choke on while I drove down the road. It gagged him and once again, he brought up the entire contents of his tummy. All over the back of the car. I couldn't get him to talk to me so I began lane changing frantically planning a straight shot to the town's emergency room which was 6 blocks away. I yelled for him to talk. He couldn't because he was to busy heaving. I finally saw a gasp of air. Then another. Then another. Then the car smelled like a someone rode the merry go round to long. If I have to be around barf another second , I am gonna lose it.
Well not really. But I am growing tired of it. A little buck naked action in a parking lot at the grocery store to change clothes. Ran in bought paper towels and 409 cleaner to so some damage control in the back seat. It was interesting he had a hard time walking around, grapping at his legs periodically saying his legs hurt.
Later at physical therapy he definitely was crabby. He was not cooperating with any body that day. She tried stretching him out and said his range of motion seems good today but he is also tender to the touch he seems like. She made a comment to me that when he doesn't want to do a certain task, he says he is tired. If it is something he enjoys then he does it no problem. I wasn't sure how to take that. I mean, it is true. But don't we all? I already knew this about him. Gary's brother and sister are the same way. Something they don't enjoy, well, let the drama roll. He does not however, fake anything. I don't think she was implying that but unfortunately after a long weekend in the hospital, a long day, I must have been sensitive.
Tomorrow we have to go back. I really don't want too. I even contemplated asking for a reschedule for later in the week. I can only imagine how Gary feels about it. He needs to be followed though. He needs his treatments to make sure we are staying in front of the JDM or extinguishing fires from this nasty bug. Five days of not being right. One thing we have to look forward to tomorrow is before we go to the floor to start his IV and get meds going, we are meeting PT at the pool. She is going to do some work in the pool.
He is in good spirits, so I am grateful. Tired but grateful.
DAD GOING DOWN
Since it was the weekend, it was nice to have my husband with me finally. Well until the IV was started. My husband was holding his hand while Gary screamed, when his head went down. The nurse called over to him, "ARE YOU OK SIR". He was pale and spinning. We told him to sit. It distracted Gary for sure but we thought Dad was going to hit the floor. It took him about ten minutes for the color to return to his face. This is the first time a relative has had this reaction. My niece did the same thing. Oh boy.
WHAT MAKES ME SAD
The happy boy is gone. He was here when the antibiotics were in his system. So was his strength. His strange euphoric happiness we just couldn't get enough of. He was good hearted, loving, caring, amazingly happy. He is back to the ornery, inpatient, not on top of the world kid. I have even asked the doctors, why? Why is that? Why is this guy back? Not saying I want to run antibiotics but it just seems funny to me.
Thursday, May 17, 2012
Can't Keep Him Down
It's hard to keep a five year old down. I know that is a good thing, but still.
Gary had a quick steroid pulse yesterday. It was methotrexate day as well. So instead of an injection, they just put it through his IV to spare a poke. Whenever they get a good vein, he can taste everything they push through the IV. We went to the park after the infusion. (Get him out, change it up, make him feel better). The whole time he kept gagging. He'd be playing on the slide, make a random sound like lunch was on its way back up. I kept asking him if he wanted to go. NO. Finally I convinced him by telling him I was going home, he could stay at some random park by himself. He took a long nap on the way home. The nap continued to the couch. He was miserable when he woke up. He couldn't stand without getting light headed which was making him beyond mad. I gave him tylenol, zofran, he was out the door. He was very emotional and not feeling well. I guess this surprised me because he has felt a lot better getting a lot more and longer of an infusion before. I was wondering if maybe the methotrexate being put right into his blood stream verses being injected made a difference.
Distraction technique number one: combining baking soda and vinegar in a bottle which was neat for oh, thirty seconds. We decided to take him to the lake for a distraction. The weather has been nice but cool weather was rolling in. At 8:30 pm, there he was, sitting in the freezing cold water in the lake, refusing to get out. He cried and said he found a warm spot, it felt so good. We live in WA, temps are still very cool, even the air. I find myself getting frustrated because as a mother, who in there right mind who let there healthy five year old soak in a cold lake as the sun goes down. Oh but there is me. I told him FINE, freeze your butt off then! His color went from wispy cloud to eggshell white. (Yes, that is the color of wall paints but work with me here, trying to give you a good description). Don't need to judge. I am too busy judging myself.
I do get his elbows and knees are starting to bother him here and there. The calcium deposits did shrink with recent treatments, but his elbows look larger to me. It could be from the steroid weight but it doesn't look like it. They seem more solid. He has even randomly complained about feeling a pinching.
It is amazing how the steroids work fast. His walk and strength will quickly improve, even later that day. We are working hard with physical therapy to try and get him as ready for Kindergarden as we can. Next week we have our big infusion. Cytoxan, Pamidronate, steroid pulse, and the return of IVIG. Should be interesting. Our physical therapist mention she may try and get him some pool time. Hopefully we can do this before he is admitted. He would really love that. We are under orders to stretch. Lots of stretching. She stretched him out on Tuesday. He was crying it hurt. But after she was done, there was a difference in his gait.
I still worry a little. At the end of the day he will walk in looking as if his body is using everything it has to make those legs go. We definitely see good days, and we also see days where he acts like he is too tired to talk. JDM has a war on its hands! Come on meds, keep punching for him.
Gary had a quick steroid pulse yesterday. It was methotrexate day as well. So instead of an injection, they just put it through his IV to spare a poke. Whenever they get a good vein, he can taste everything they push through the IV. We went to the park after the infusion. (Get him out, change it up, make him feel better). The whole time he kept gagging. He'd be playing on the slide, make a random sound like lunch was on its way back up. I kept asking him if he wanted to go. NO. Finally I convinced him by telling him I was going home, he could stay at some random park by himself. He took a long nap on the way home. The nap continued to the couch. He was miserable when he woke up. He couldn't stand without getting light headed which was making him beyond mad. I gave him tylenol, zofran, he was out the door. He was very emotional and not feeling well. I guess this surprised me because he has felt a lot better getting a lot more and longer of an infusion before. I was wondering if maybe the methotrexate being put right into his blood stream verses being injected made a difference.
Distraction technique number one: combining baking soda and vinegar in a bottle which was neat for oh, thirty seconds. We decided to take him to the lake for a distraction. The weather has been nice but cool weather was rolling in. At 8:30 pm, there he was, sitting in the freezing cold water in the lake, refusing to get out. He cried and said he found a warm spot, it felt so good. We live in WA, temps are still very cool, even the air. I find myself getting frustrated because as a mother, who in there right mind who let there healthy five year old soak in a cold lake as the sun goes down. Oh but there is me. I told him FINE, freeze your butt off then! His color went from wispy cloud to eggshell white. (Yes, that is the color of wall paints but work with me here, trying to give you a good description). Don't need to judge. I am too busy judging myself.
I do get his elbows and knees are starting to bother him here and there. The calcium deposits did shrink with recent treatments, but his elbows look larger to me. It could be from the steroid weight but it doesn't look like it. They seem more solid. He has even randomly complained about feeling a pinching.
It is amazing how the steroids work fast. His walk and strength will quickly improve, even later that day. We are working hard with physical therapy to try and get him as ready for Kindergarden as we can. Next week we have our big infusion. Cytoxan, Pamidronate, steroid pulse, and the return of IVIG. Should be interesting. Our physical therapist mention she may try and get him some pool time. Hopefully we can do this before he is admitted. He would really love that. We are under orders to stretch. Lots of stretching. She stretched him out on Tuesday. He was crying it hurt. But after she was done, there was a difference in his gait.
I still worry a little. At the end of the day he will walk in looking as if his body is using everything it has to make those legs go. We definitely see good days, and we also see days where he acts like he is too tired to talk. JDM has a war on its hands! Come on meds, keep punching for him.
Thursday, May 10, 2012
Rituxan Infusion
It became clear to me that by Sunday, maybe Monday morning, we should not have skipped that steroid pulse on Wednesday. His limp kept coming in and out, the good ol' red rash on his face returned.
Tuesday we had a physical therapy. We love our physical therapist. She is knowledgeable, and does well dealing with Gary. His reports came back and it was what we expected. Below average to well below average for bilateral coordination and balance. So the plan is as soon as he is to a infusions once a month we well step up therapy. We are hoping this summer to do twice a week, and occupational therapy, like hand strengthening ect,.
When I told our doctor that I think we should have went ahead and pulsed him last week, she brought up one more time, the port. She warned me that this was the last time she would mention it. She said that she is not in favor of it, but if I am, then she will put the order in. Because it looks like we are going to go to once a week infusions for a little bit here. I said no. Then we had a 5 poke infusion start.
Just going with it right now. Making sure he stays walking and swallowing. Making sure I stay in tune with his symptoms. Tired.
Tuesday we had a physical therapy. We love our physical therapist. She is knowledgeable, and does well dealing with Gary. His reports came back and it was what we expected. Below average to well below average for bilateral coordination and balance. So the plan is as soon as he is to a infusions once a month we well step up therapy. We are hoping this summer to do twice a week, and occupational therapy, like hand strengthening ect,.
When I told our doctor that I think we should have went ahead and pulsed him last week, she brought up one more time, the port. She warned me that this was the last time she would mention it. She said that she is not in favor of it, but if I am, then she will put the order in. Because it looks like we are going to go to once a week infusions for a little bit here. I said no. Then we had a 5 poke infusion start.
Just going with it right now. Making sure he stays walking and swallowing. Making sure I stay in tune with his symptoms. Tired.
Saturday, May 5, 2012
Wednesday Clinic
We packed to stay the night, but with a new doctor comes changes. She is different from our other doctor. Thinks out loud. Thats ok. But it does spin me a bit. We packed for IVIG and a steroid pulse. Which means we packed to possibly stay overnight. But just the same we were going to be admitted.
Good news is he is doing better. Well enough to skip this weeks steroid pulse intravenously. His limp from his hip improved a lot. When he runs, you can hear it, barely see it. Means? Means I can hear a quick thump thump. A regular run is a step one right after the other, in rhythm. His is more of a one two one two one two. So the whole hip lag drap thing is so much better. I have seen little to no evidence of swallowing issues. It does not help he came down with a bad cold Friday. I was surprised they weren't more concerned. But with no fever, energy in steroid Zone, can't treat something that is not there. He has lost his voice from the cold so the doctor was not pleased with the quality, but he has a cold.
Remicade
So they stopped Remicade. They orginally started Remicade not to treat JDM but to treat his colon. The speculation that the Remicade might be making him flare. Agree. Not entirely.
So we held IVIG. Part of me thinks she is still going to cut it out completely. We return next week for the next dose of Rituxan and a steroid pulse. That will be all with the Rituxan for another 4-6 months.
The next week after that we return for another overnight of Cytoxan, IVIG, Pamidronate, and steroids.
We were sent home to come back next Wednesday.
Friday (5/4) we had an emergency dentist appointment. The day before Gary woke up to what appeared to be a toothache. He was rolling around on my bed at 6am, crying his tooth hurt. I immediately gave him tylenol and called the dentist. It was 7am and they were there. I couldn't believe. Gary also see's Children's Hospital in Seattle Dentistry Department. They deal with immune compromised children. There is a certain special handling these kids need. They got us in at 10am. The dentist saw no immediate evidence of an abscess. But he does have a few cavities. Gary is to young for xrays. The dentist was very nervous so she talked to me about putting him completely under to take care of everything. They will put him under general anesthesia. Do xrays, fillings, cleaning, ect,. I know what you are thinking. For a dentist? Really is it necessary? Yes. It is. Gary has had extensive medical procedures that have made him intolerant. Extremely intolerant. That was evident during the MRI we tried to get him to do without sedation. The dentist was even more concerned and motivated to get an xray done when she saw he was on pamidronate infusions. She explained how these infusions can change the composition of his bones. She said his baby teeth might not fall out the way they should because of the strength this creates in the bones. Good add another to the list. So he will be getting some sleepy juice. She said it was important to make sure he doesn't have necrosis in the jaw from the pamidronate. This means the bones dies. It has not been seen in children, but has in adults. I love it when it is explained to me, "we are exploring new horizons with this treatment and how it effects dental bone development." Oh how fun.
He is still trying to recover from a cold he caught. He has had it for 8 days now. But it doesn't make him feel bad or sleep bad, so that is a plus. His heliotrope rash is there on and off. It is faint enough someone who doesn't know him will say he looks good.
Good news is he is doing better. Well enough to skip this weeks steroid pulse intravenously. His limp from his hip improved a lot. When he runs, you can hear it, barely see it. Means? Means I can hear a quick thump thump. A regular run is a step one right after the other, in rhythm. His is more of a one two one two one two. So the whole hip lag drap thing is so much better. I have seen little to no evidence of swallowing issues. It does not help he came down with a bad cold Friday. I was surprised they weren't more concerned. But with no fever, energy in steroid Zone, can't treat something that is not there. He has lost his voice from the cold so the doctor was not pleased with the quality, but he has a cold.
Remicade
So they stopped Remicade. They orginally started Remicade not to treat JDM but to treat his colon. The speculation that the Remicade might be making him flare. Agree. Not entirely.
So we held IVIG. Part of me thinks she is still going to cut it out completely. We return next week for the next dose of Rituxan and a steroid pulse. That will be all with the Rituxan for another 4-6 months.
The next week after that we return for another overnight of Cytoxan, IVIG, Pamidronate, and steroids.
We were sent home to come back next Wednesday.
Friday (5/4) we had an emergency dentist appointment. The day before Gary woke up to what appeared to be a toothache. He was rolling around on my bed at 6am, crying his tooth hurt. I immediately gave him tylenol and called the dentist. It was 7am and they were there. I couldn't believe. Gary also see's Children's Hospital in Seattle Dentistry Department. They deal with immune compromised children. There is a certain special handling these kids need. They got us in at 10am. The dentist saw no immediate evidence of an abscess. But he does have a few cavities. Gary is to young for xrays. The dentist was very nervous so she talked to me about putting him completely under to take care of everything. They will put him under general anesthesia. Do xrays, fillings, cleaning, ect,. I know what you are thinking. For a dentist? Really is it necessary? Yes. It is. Gary has had extensive medical procedures that have made him intolerant. Extremely intolerant. That was evident during the MRI we tried to get him to do without sedation. The dentist was even more concerned and motivated to get an xray done when she saw he was on pamidronate infusions. She explained how these infusions can change the composition of his bones. She said his baby teeth might not fall out the way they should because of the strength this creates in the bones. Good add another to the list. So he will be getting some sleepy juice. She said it was important to make sure he doesn't have necrosis in the jaw from the pamidronate. This means the bones dies. It has not been seen in children, but has in adults. I love it when it is explained to me, "we are exploring new horizons with this treatment and how it effects dental bone development." Oh how fun.
He is still trying to recover from a cold he caught. He has had it for 8 days now. But it doesn't make him feel bad or sleep bad, so that is a plus. His heliotrope rash is there on and off. It is faint enough someone who doesn't know him will say he looks good.
Friday, April 27, 2012
Monday Turned It All Around
So after Friday's appointment and joyfully skipping home that we didn't have to stay there. We knew we would be coming back Monday but still was good to go home. The weekend was good. Great weather. Saturday we had Elexis's final soccer game. Sunday we went to a Relay Race out in North Bend. Fun. Monday we checked in at clinic at 10:30am. It was definitely hard to roll out of bed for everyone after the busy weekend.
Not much had changed with Gary from Friday. The doctor took the time to do a CMAS test. We typically don't do those because of his age. But now that he is older she wanted to get a baseline. I did bring up the swallowing thing again. Over the weekend his coughing while eating started to increase. Drinking from a water bottle triggered a cough/wheeze pull over the car are you ok incident. The family mention they noticed more and more something seemed off. I didn't emphasize it. Only mentioned it because of the doctors reaction from it on Friday. She by no means dismissed it, but maybe could have taken the time to listen closely. However, it was the first day we noticed something so we didn't have enough times to support warranting a test. Again, she said brushed it away. His hoarse voice turned a little nasally sounding as well. She did noticed that but during a speech pronouncing test, he seemed to have no trouble.
After the appointment we headed to the floor for admitting to get the ball rolling. We had to share a room but our roommate was an wonderful. A little peanut of a baby who made little sound because he couldn't. The resident doctor came in to meet and greet. They are responsible for putting in all the orders of medications. It is basically like have 2 clinic appointments in a row. Sometimes I will forget things because I already went over it in clinic less than 20 minutes before that. The beauty of it however is with the resident doctors. They can be difficult to deal with but will order tests. I explained to her what we have been seeing. She said, "let's order a bed side speech consult." Speech consults also evaluate swallowing. Later that day she arrived with a plate of food. Yogurt, bagel, chips, and juice. She was familiar with Gary. I recognized her from when his swallowing was effected at the beginning of his diagnosis. We started out with the yogurt. Right away we both looked at each other as he grabbed his nose, his eyes watered, and he sniffed. The rest of the food he did fine with. Like in the past week, it wasn't all the time, just hear and there. Signs. After her evaluation she said he definitely needed a swallow test done. She said she is seeing obvious signs including the food would change the sound of his voice. This indicates his muscles aren't clearing the food completely.
MRI Try
Before speech came down to our room, the resident suggested we try giving him an MRI without sedation, totally awake. Well, ok, I guess. So that is what we tryed. We barely got to the door of the MRI room and he started to become very upset. Eye roll. Please people. In the past month he has had a colonscopy, an endocscopy, a spinal tap, repeated IV starts and blood draws. My child isn't easy going like that when it comes to things like this. I don't blame him. Even giving it a try was not necessary. No need to cause undo stress. Of course I let them try because it would just be once less thing that goes into his body. I admit I hoped it would work out too.
The MRI was the next morning because he need to have nothing in his tummy. Placing him on the table to be sedated was just as bad. Anything that runs through his IV is always sensitive. He ouches and gasps. They explained the sedation med can sting pretty bad. They try and put some numbing stuff in to help but it didn't. As soon as the milky white liquid was pushed into his IV he went into hysterics. He started to bang his head and flip his body back and forth in agony. Less than ten seconds later he was snoring. He quickly drifted back, we layed him into place. An hour and a half later he was out again.
CONVERSATIONS With the doctor
After the medical team received the evaluation about the swallowing, our rheumatologist popped in. She looked a little.....not mad....but maybe frustrated and couldn't believe it. "So its real, that is what you were really seeing." She shook her head then proceeded to dive into her own mind. We kept going over the what he has had, when he had, the order of the past couple months. She said she was very displeased with the swallowing. She stepped into the room and said, "so its real." She went over medications. Suddenly we were adding drugs back on the list. Including IVIG and Rituxan. She admitted she was scared to give him this combination. We talked about more steroids. Going back up on the home dose. Questions and answers bounced back and forth between her and I. The port word even came into the picture. Weekly steroid pulses until he recovers. The main anxiety she was having was Rituxan and Remicade and Cytoxan. The MRI done the next morning did confirm the funny limp was from inflammation.
The good news is he passed his swallow test. That means when they were taking live video under Xray of him swallowing, all seemed fine like I said. I wondered with those results if that changed things. Like maybe she would want to hold off on running the Rituxan. The doctors came in and said no. They wanted to proceed. I needed time. So I asked that they give him his steroid pulse that night then run the Rituxan so I could really decide if this is what was best. It was a plunge kind of decision. Just do? My reasoning came down to this, He was due for his 4 month mark of the Rituxan dose. I did not think with the results of stopping the cell cept, tacrolimus, and enbrel, we dare not stop another medication. Even later that evening one rheumatologist came in and wanted to talk. She said they called an expert who had recommended the Enbrel shots. A point was made regarding the Remicade. There are a few case studies in adults where the Remicade actually made dermatomyositis worse. They wanted to know what I thought. Right now I think no. I don't think remicade is responsible for this sudden muscles weaknesses. I think its the JDM protocal taper effect. < I just made that up sort of.) But with this disease, taper is the name of the game. And the doctors know that. They also suggested it could be from going from 5ml to 3ml in a matter of weeks. Gary has proven to be sensitive to steroids. When on and trying to go off them. Still unknown. I think the most important thing is that we need to bring the inflammation back under control. One of the most agitating things, Gary's labs are not bad at all. We can say that is good? But labs never tell whole tale.
Gary is home and doing great. His breath smells bad from all the medication. They put him back on fluconzole for thrush. Not even hours after Cytoxan was finished, thrush appeared in his mouth.
It's twisted and complicated. Just want him to keep smiling. I will take care of everything else.
Not much had changed with Gary from Friday. The doctor took the time to do a CMAS test. We typically don't do those because of his age. But now that he is older she wanted to get a baseline. I did bring up the swallowing thing again. Over the weekend his coughing while eating started to increase. Drinking from a water bottle triggered a cough/wheeze pull over the car are you ok incident. The family mention they noticed more and more something seemed off. I didn't emphasize it. Only mentioned it because of the doctors reaction from it on Friday. She by no means dismissed it, but maybe could have taken the time to listen closely. However, it was the first day we noticed something so we didn't have enough times to support warranting a test. Again, she said brushed it away. His hoarse voice turned a little nasally sounding as well. She did noticed that but during a speech pronouncing test, he seemed to have no trouble.
After the appointment we headed to the floor for admitting to get the ball rolling. We had to share a room but our roommate was an wonderful. A little peanut of a baby who made little sound because he couldn't. The resident doctor came in to meet and greet. They are responsible for putting in all the orders of medications. It is basically like have 2 clinic appointments in a row. Sometimes I will forget things because I already went over it in clinic less than 20 minutes before that. The beauty of it however is with the resident doctors. They can be difficult to deal with but will order tests. I explained to her what we have been seeing. She said, "let's order a bed side speech consult." Speech consults also evaluate swallowing. Later that day she arrived with a plate of food. Yogurt, bagel, chips, and juice. She was familiar with Gary. I recognized her from when his swallowing was effected at the beginning of his diagnosis. We started out with the yogurt. Right away we both looked at each other as he grabbed his nose, his eyes watered, and he sniffed. The rest of the food he did fine with. Like in the past week, it wasn't all the time, just hear and there. Signs. After her evaluation she said he definitely needed a swallow test done. She said she is seeing obvious signs including the food would change the sound of his voice. This indicates his muscles aren't clearing the food completely.
MRI Try
Before speech came down to our room, the resident suggested we try giving him an MRI without sedation, totally awake. Well, ok, I guess. So that is what we tryed. We barely got to the door of the MRI room and he started to become very upset. Eye roll. Please people. In the past month he has had a colonscopy, an endocscopy, a spinal tap, repeated IV starts and blood draws. My child isn't easy going like that when it comes to things like this. I don't blame him. Even giving it a try was not necessary. No need to cause undo stress. Of course I let them try because it would just be once less thing that goes into his body. I admit I hoped it would work out too.
The MRI was the next morning because he need to have nothing in his tummy. Placing him on the table to be sedated was just as bad. Anything that runs through his IV is always sensitive. He ouches and gasps. They explained the sedation med can sting pretty bad. They try and put some numbing stuff in to help but it didn't. As soon as the milky white liquid was pushed into his IV he went into hysterics. He started to bang his head and flip his body back and forth in agony. Less than ten seconds later he was snoring. He quickly drifted back, we layed him into place. An hour and a half later he was out again.
CONVERSATIONS With the doctor
After the medical team received the evaluation about the swallowing, our rheumatologist popped in. She looked a little.....not mad....but maybe frustrated and couldn't believe it. "So its real, that is what you were really seeing." She shook her head then proceeded to dive into her own mind. We kept going over the what he has had, when he had, the order of the past couple months. She said she was very displeased with the swallowing. She stepped into the room and said, "so its real." She went over medications. Suddenly we were adding drugs back on the list. Including IVIG and Rituxan. She admitted she was scared to give him this combination. We talked about more steroids. Going back up on the home dose. Questions and answers bounced back and forth between her and I. The port word even came into the picture. Weekly steroid pulses until he recovers. The main anxiety she was having was Rituxan and Remicade and Cytoxan. The MRI done the next morning did confirm the funny limp was from inflammation.
The good news is he passed his swallow test. That means when they were taking live video under Xray of him swallowing, all seemed fine like I said. I wondered with those results if that changed things. Like maybe she would want to hold off on running the Rituxan. The doctors came in and said no. They wanted to proceed. I needed time. So I asked that they give him his steroid pulse that night then run the Rituxan so I could really decide if this is what was best. It was a plunge kind of decision. Just do? My reasoning came down to this, He was due for his 4 month mark of the Rituxan dose. I did not think with the results of stopping the cell cept, tacrolimus, and enbrel, we dare not stop another medication. Even later that evening one rheumatologist came in and wanted to talk. She said they called an expert who had recommended the Enbrel shots. A point was made regarding the Remicade. There are a few case studies in adults where the Remicade actually made dermatomyositis worse. They wanted to know what I thought. Right now I think no. I don't think remicade is responsible for this sudden muscles weaknesses. I think its the JDM protocal taper effect. < I just made that up sort of.) But with this disease, taper is the name of the game. And the doctors know that. They also suggested it could be from going from 5ml to 3ml in a matter of weeks. Gary has proven to be sensitive to steroids. When on and trying to go off them. Still unknown. I think the most important thing is that we need to bring the inflammation back under control. One of the most agitating things, Gary's labs are not bad at all. We can say that is good? But labs never tell whole tale.
Gary is home and doing great. His breath smells bad from all the medication. They put him back on fluconzole for thrush. Not even hours after Cytoxan was finished, thrush appeared in his mouth.
It's twisted and complicated. Just want him to keep smiling. I will take care of everything else.
Wednesday, April 18, 2012
I'm in a spin, Not loving the spin I am in.....
Today, April 18th, was our clinic and cytoxan admission. Well, it was suppose to be. Our appointment was at 2:15. Gary weighed in at 46 pounds. That is seven pounds in 2 weeks. It certainly looks like a whole lot more but it is temporary. His energy is off the charts. So far off the charts his body isn't keeping up with him. After physical therapy on Thursday last week, his walk went to a limp drag. He hobbles horribly. Complains of no pain, just hobbles faster. The limp drag and sudden drastic weight gain, reminds me of Quazie Motto. His attitude remains above the clouds. Above anyone else's on earth. He is so very happy. A few unnatural tantrums have crept in but those far outweigh his sunny disposition that we have not seen. I couldn't paint a picture with words for our doctor. Saying he is a new kid doesn't do it.
We went through the regular conversation. Fevers, no. Sleeping well. All is well. One little detail that I discovered that morning was swallowing. During Gary's birthday celebration with the family we video taped him while he ate dinner. I was watching the video and noticed he was grabbing his throat when the food went down his throat. At the time I noticed but just stored it in my memory. My memory was tapped into this afternoon before we left. He was eating chicken nuggets. I glanced out of the side of eyes and saw him grab his throat and wince. I asked what was wrong. He said the food won't go down. No choking. No coughing. Why is it almost painful when things are dismissed? Not listening. Dismissing to quickly. Moving to fast. Frustrating. It is a scenario that has played out to many times during the past three years. Mothers are to be listened too. This to shall come to past. If I was the doctor, I understand. I am looking at a child that has gained weight, there is no trouble with food making it to his stomach. This new, as is his limp. His limp isn't just any limp, its a JDM limp, neither is his swallowing. Not related. Especially being pulled off five different medications he has been on for a long time. I just have to breathe, when I really want to scream. I know it seems ironic to most people when he is feeling so much better. Good, doesn't take away the fact that we have just come of a flare, blood infection, and major med changes followed by symptoms. Oh what fun! > : (
MEDICATION
In order to get our infusion down to once a month, we came home tonight. We are returning Monday night for Cytoxan, Pamidronate, and Remicade. Remicade is a little early, but just this once, too get these to line up. Our new rheumatologist decided to also discontinue his Rituxan infusions. She felt they aren't working. On a recent trip overseas and some convention, it was discussed how there particular country doesn't use Ritxuan. There was some confusion between the doctor and I. We had previously talked about Remicade being used for JDM. Traditionally it is used for IBD. So she asked me to ask my JDM Mom's if anyone was on Remicade for JDM. So I did. Not many. She walked into todays appointment asking about Rituximab which is Rituxan. She told me they don't use this medication over there. I would love to through out a so what! right here but I know I don't know the whole story and her whole point. This will all be cleared up. This appointment was like being on a merry go round that wouldn't stop. This transition is proving to be a tough one.
Coming down to 3ml on steroids though. She ordered a MRI on Monday of his hip to check for necrosis which I heard can happen with high dose steroids. We are gonna steer clear of the internet until after that MRI on Monday. No reason to get myself all worked up. I already am. I am thankful he is doing well and better and all that. It doesn't take my fight away. It does make it easier. I almost typed it doesn't but really if was very sick or in bad pain, well then, it would be much harder. My favorite! Perspective.
Now it seems to me that our doctor is going after these calcium deposits. They are looking much better so that is a good thing. Just have to tackle the rest, not just one thing. I know the doctor realizes this but the whole oh yay, alright, thing just erks me. You can break it down, explain it, try and help me with my feelings but until you walk in it or even at that, no one can ever put my shoes on, they don't fit.
WHAT IS WORKING, WHAT WAS WORKING?
Gary's Medications
3ml Prednisone
2.25ml Cellcept
2.5ml Tacrolimus
1/2 tab of Hydroxychloroquine
.75ml Methotrexate Injections
25mgs Enbrel Injections
IVIG Infusions
Rituxan Infusions
.8 Enalapril
Folic Acid
Calcium/Vit D
MultiVitamin
ADDED:
Cytoxan Infusions
Remicade Infusions
5ml Raninadine
Do I approve. That is what I was asked. I think taking away too many at one time is a little scary. I suppose all I can do is go with it. I asked her when she anticipates taking him off Cytoxan. She wants him to go at least for six months then we will move him to a home dose of a different immune suppression. Imuran or another she mentioned. That will bump us right into Kindergarden. If she sticks to this schedule, August will be the six month mark. I guess what I would like everyone to consider is the steroids and "how well" he is doing. He has proven to really like steroids. His body responds to prednisone. I don't want anything masked by the immediate effects of removing these medications.
BACTERIA
I asked her if she had heard anything further regarding Gary's blood infection. She did get the report that the bacteria was not found in the biopsies they took during his endoscopy and colonoscopy. She doesn't think it came from the dog. She thinks it came from an infection we saw under his skin. It was a calcium deposit or a molluscum. I have lost count of opinions.
We went through the regular conversation. Fevers, no. Sleeping well. All is well. One little detail that I discovered that morning was swallowing. During Gary's birthday celebration with the family we video taped him while he ate dinner. I was watching the video and noticed he was grabbing his throat when the food went down his throat. At the time I noticed but just stored it in my memory. My memory was tapped into this afternoon before we left. He was eating chicken nuggets. I glanced out of the side of eyes and saw him grab his throat and wince. I asked what was wrong. He said the food won't go down. No choking. No coughing. Why is it almost painful when things are dismissed? Not listening. Dismissing to quickly. Moving to fast. Frustrating. It is a scenario that has played out to many times during the past three years. Mothers are to be listened too. This to shall come to past. If I was the doctor, I understand. I am looking at a child that has gained weight, there is no trouble with food making it to his stomach. This new, as is his limp. His limp isn't just any limp, its a JDM limp, neither is his swallowing. Not related. Especially being pulled off five different medications he has been on for a long time. I just have to breathe, when I really want to scream. I know it seems ironic to most people when he is feeling so much better. Good, doesn't take away the fact that we have just come of a flare, blood infection, and major med changes followed by symptoms. Oh what fun! > : (
MEDICATION
In order to get our infusion down to once a month, we came home tonight. We are returning Monday night for Cytoxan, Pamidronate, and Remicade. Remicade is a little early, but just this once, too get these to line up. Our new rheumatologist decided to also discontinue his Rituxan infusions. She felt they aren't working. On a recent trip overseas and some convention, it was discussed how there particular country doesn't use Ritxuan. There was some confusion between the doctor and I. We had previously talked about Remicade being used for JDM. Traditionally it is used for IBD. So she asked me to ask my JDM Mom's if anyone was on Remicade for JDM. So I did. Not many. She walked into todays appointment asking about Rituximab which is Rituxan. She told me they don't use this medication over there. I would love to through out a so what! right here but I know I don't know the whole story and her whole point. This will all be cleared up. This appointment was like being on a merry go round that wouldn't stop. This transition is proving to be a tough one.
Coming down to 3ml on steroids though. She ordered a MRI on Monday of his hip to check for necrosis which I heard can happen with high dose steroids. We are gonna steer clear of the internet until after that MRI on Monday. No reason to get myself all worked up. I already am. I am thankful he is doing well and better and all that. It doesn't take my fight away. It does make it easier. I almost typed it doesn't but really if was very sick or in bad pain, well then, it would be much harder. My favorite! Perspective.
Now it seems to me that our doctor is going after these calcium deposits. They are looking much better so that is a good thing. Just have to tackle the rest, not just one thing. I know the doctor realizes this but the whole oh yay, alright, thing just erks me. You can break it down, explain it, try and help me with my feelings but until you walk in it or even at that, no one can ever put my shoes on, they don't fit.
WHAT IS WORKING, WHAT WAS WORKING?
Gary's Medications
3ml Prednisone
1/2 tab of Hydroxychloroquine
.75ml Methotrexate Injections
.8 Enalapril
Folic Acid
Calcium/Vit D
MultiVitamin
ADDED:
Cytoxan Infusions
Remicade Infusions
5ml Raninadine
Do I approve. That is what I was asked. I think taking away too many at one time is a little scary. I suppose all I can do is go with it. I asked her when she anticipates taking him off Cytoxan. She wants him to go at least for six months then we will move him to a home dose of a different immune suppression. Imuran or another she mentioned. That will bump us right into Kindergarden. If she sticks to this schedule, August will be the six month mark. I guess what I would like everyone to consider is the steroids and "how well" he is doing. He has proven to really like steroids. His body responds to prednisone. I don't want anything masked by the immediate effects of removing these medications.
BACTERIA
I asked her if she had heard anything further regarding Gary's blood infection. She did get the report that the bacteria was not found in the biopsies they took during his endoscopy and colonoscopy. She doesn't think it came from the dog. She thinks it came from an infection we saw under his skin. It was a calcium deposit or a molluscum. I have lost count of opinions.
Friday, April 13, 2012
Getting It All Sorted Out
Gary is doing great. Last week, on Thursday, we went Easter shopping. As I lifted him out of the car I noticed his lips looked chapped. It is not the normal dry lip kind. It's like his lip blister on the inside. I was overly concerned but the thought of "this isn't over" entered my mind. Fifteen minutes later they called. The doctor explained they wanted to continue to treat him with antibiotics. They call it triple therapy. Two antibiotics with a high dose acid reducer. He spoke fast and I tried to remember everything he said. I thought I heard him say they had never seen this particular bacteria in the blood before. The next day Gary has his Remicade infusion (Friday). He did well. It was a two hour infusion so we were their for five hours. He had a little trouble with blood pressure but nothing terrible. We had an appointment in Seattle to follow-up with his GI specialist. Gary was in no mood to be there. We talked about how well he was doing with diarrhea. That is when he informed me that he had just gotten an email from the microbiology lab. The final ID on the bacteria is called helicobacter canis. Yes, canis, meaning dog. The GI specialist asked if we had a dog and said we should have her tested. This just sends me to a blank place. I just don't know what to say. I have looked it up on the internet and I didn't find much. Nothing that the doctor didn't find on the internet during our appointment. I suppose the good part is that this blood infection is treatable. Like before it complicates things. The GI doctor told me he is almost positive that the ulcers they found in his colon were not from this bacteria. He thinks they were medication induced. Whether or not he has IBD he doesn't know. He wants to continue to run the Remicade for at least the next six months. See how he is doing then decide if we can stop. He warned of reactions the body can have after being of Remicade and coming off it. He said it will likely not happen. I have so many questions that no one can answer because they don't know. Like:
When we came into ER on Monday with a fever, headache, and vomiting, was that from this blood infection or from the IVIG? And if it is not from the IVIG, are we going to keep getting IVIG or are they pulling it from his infusions? As soon as they gave antibiotics, he started feeling so much better. How would antibiotics help aseptic meningitis from the IVIG? They wouldn't? Seems he had multiply things going on. Now that he has had 4 different antibiotics, cytoxan, remicade, steroid increase, it is hard to tell where his JDM falls into this.
Gary responded so well to the antibiotics. I mean, he is really a different kid. Despite going back up on steroids, he seems so joyful. He is wonderful to be around, so full of love and happiness. Seeing this side of him, he was not before all this happened with the blood infection. His energy is wonderful. He is eating a whole lot and the effects of the steroids can be seen in his face and tummy but I looooovvveee it. I love hugging him and kissing his cheeks. The steroid temper is not really there. He is just this new child. We finally got to start physical therapy. They tested him last week and this week. The scores indicated exactly what we see. A bilateral balance weakness, he fell way below average. It is nothing I didn't expect though. His coordination seem very good. He was average with ball catching and that sort of thing. Yesterday they tested his fine motor skills. He was instructed to color in a small circle and and a small star with a red color pencil. He used a lot of concentration. He is so very cute. He put maximum effort in. At one point he was getting frustrated going outside the like. He placed his finger down at the line to stop the pencil from going over the line. She noted he gets fatigued easily. I noticed that as well. He was huffing and puffing just completely the tasks. But I was very proud of him. Seeing him sitting there using scissors and folding paper. It was like a little message that he is going to do great in Kindergarten. She decided to test his grip strength. The more he did, the littler then pencil drawing became. It was based upon a 6 year old but, the average for a six year old is 30 lbs. Gary was squeezing no more than 2 lbs with all his might. No biggie, just going to get him working his hands. My hope is to have him good for September 2012. There are issues with immunizations that we have to get worked out with the doctors. As soon as his treatment is over for the bacteria infection we can proceed. The physical therapy is something I am so glad he is getting. He really did need it. All the ability is there. She made a comment to me, if we can just get him feeling confidant. Until he gets those balance muscles recovered we just need to keep building him up. She set out a small trampoline for him to jump on. He promptly got on it and began to jump, assisted. He tired and asked to get down. She said sure. He sat to his bottom and scooted off. She said lets try that again. She had him step back up, and step back down. He did it with her assistance. The whole workout had the poor guy limping out. But what was amazing was his attitude and wanting to keep going on with his day.
March and April have definitely proved to be interesting so far. I am liking so much how well he is responding to his medications, on a JDM level and for the infection. I do anticipate a honeymoon phase getting back together with Cytoxan and with Remicade in the picture he has always responded well at first. I pray it keeps going this time. If it doesn't, it doesn't. We will keep working at it. Gary's calcinosis is looking good. His pamidronate infusion have beeen moved to once a month but we have not done the back to back as of yet so maybe there won't be a need for it. He is going to be getting a lot of infusions over the next couple weeks. I have seen some signs of vasculitis under his armpits and across his tummy and chest. But it goes in and out. Time for sunblock again around here : )
Thank you to my very special friends Lynn Williams, The Marcotte Family, and Sue Carpentar for send special gifts making our stay in the hospital fun. Thank you to my baby sister who is there at a moments notice for any and everything we need. Thank you to Grandma's and Grandpa for visiting. Thank you to the Saas Family for spending Saturday with us. You are all so very very special to us.
When we came into ER on Monday with a fever, headache, and vomiting, was that from this blood infection or from the IVIG? And if it is not from the IVIG, are we going to keep getting IVIG or are they pulling it from his infusions? As soon as they gave antibiotics, he started feeling so much better. How would antibiotics help aseptic meningitis from the IVIG? They wouldn't? Seems he had multiply things going on. Now that he has had 4 different antibiotics, cytoxan, remicade, steroid increase, it is hard to tell where his JDM falls into this.
Gary responded so well to the antibiotics. I mean, he is really a different kid. Despite going back up on steroids, he seems so joyful. He is wonderful to be around, so full of love and happiness. Seeing this side of him, he was not before all this happened with the blood infection. His energy is wonderful. He is eating a whole lot and the effects of the steroids can be seen in his face and tummy but I looooovvveee it. I love hugging him and kissing his cheeks. The steroid temper is not really there. He is just this new child. We finally got to start physical therapy. They tested him last week and this week. The scores indicated exactly what we see. A bilateral balance weakness, he fell way below average. It is nothing I didn't expect though. His coordination seem very good. He was average with ball catching and that sort of thing. Yesterday they tested his fine motor skills. He was instructed to color in a small circle and and a small star with a red color pencil. He used a lot of concentration. He is so very cute. He put maximum effort in. At one point he was getting frustrated going outside the like. He placed his finger down at the line to stop the pencil from going over the line. She noted he gets fatigued easily. I noticed that as well. He was huffing and puffing just completely the tasks. But I was very proud of him. Seeing him sitting there using scissors and folding paper. It was like a little message that he is going to do great in Kindergarten. She decided to test his grip strength. The more he did, the littler then pencil drawing became. It was based upon a 6 year old but, the average for a six year old is 30 lbs. Gary was squeezing no more than 2 lbs with all his might. No biggie, just going to get him working his hands. My hope is to have him good for September 2012. There are issues with immunizations that we have to get worked out with the doctors. As soon as his treatment is over for the bacteria infection we can proceed. The physical therapy is something I am so glad he is getting. He really did need it. All the ability is there. She made a comment to me, if we can just get him feeling confidant. Until he gets those balance muscles recovered we just need to keep building him up. She set out a small trampoline for him to jump on. He promptly got on it and began to jump, assisted. He tired and asked to get down. She said sure. He sat to his bottom and scooted off. She said lets try that again. She had him step back up, and step back down. He did it with her assistance. The whole workout had the poor guy limping out. But what was amazing was his attitude and wanting to keep going on with his day.
March and April have definitely proved to be interesting so far. I am liking so much how well he is responding to his medications, on a JDM level and for the infection. I do anticipate a honeymoon phase getting back together with Cytoxan and with Remicade in the picture he has always responded well at first. I pray it keeps going this time. If it doesn't, it doesn't. We will keep working at it. Gary's calcinosis is looking good. His pamidronate infusion have beeen moved to once a month but we have not done the back to back as of yet so maybe there won't be a need for it. He is going to be getting a lot of infusions over the next couple weeks. I have seen some signs of vasculitis under his armpits and across his tummy and chest. But it goes in and out. Time for sunblock again around here : )
Thank you to my very special friends Lynn Williams, The Marcotte Family, and Sue Carpentar for send special gifts making our stay in the hospital fun. Thank you to my baby sister who is there at a moments notice for any and everything we need. Thank you to Grandma's and Grandpa for visiting. Thank you to the Saas Family for spending Saturday with us. You are all so very very special to us.
Friday, April 6, 2012
Sorry the continue as taken so long....
After a few days he only gained strength. His numbers got better. After what seemed like over of week, they were talking about sending us home. When we first returned to the ER I was assured by several medical professionals that Gary would be receiving a picc line. As much as I didn't want my little angel who had been through so much already to have to have something like this put into his body, I strangely looked forward to it. I looked forward to not having to poke him over and over again over the next couple of weeks. So on Monday when anesthesia came in and went over procedure I had come to grips, accepted it. Not five minutes later, infectious disease department walked in. What struck me as just plain arrogance they began to speak. I corrected them they had his history wrong. She explained from what she understood Gary was stopped on MMF and Tacrolimus because he was doing so well. They had started him on cytoxan and remicade to continue treating the IBD symptoms and JDM replacing the MMF and Tac. Wrong. I quickly corrected them. Not sure they were even listening to me. They quickly pointed out they were their to make sure he did not get a picc line. Ok. Spinning. Fine! Since he is doing so well they said they are more apt to treat for 24 more hours and send us home. Depending upon the infection and symptoms we had been told 10 to 14 days. Then 7 to 10. He had already gotten 6. Their recommendations were to not put in a picc line and send us home. As a mother, I want to go home, and oh one little important detail, I don't want my child to be so sick something really bad happens due to someones else's neglect. I wouldn't have it. I don't care how well he was doing or what he responded too, they still at this point did not have an id on the bug. This meant they did not know the exact way to treat it. They could guess the 2 broad spectrum antibiotics they had already put in already nailed it, but could they know for sure in a immunosuppressive 5 year old!!! Think not! Rip me in two why don't you. I couldn't figure out why they were making me angry. Who wants to stay at the hospital. I don't. But I also don't want people making assumptions.
We were discharged Monday with no picc line. Celebrate, for sure. Nervous, definitely. He continues to do well. I am so knotted up about everything I can barely breathe. Today, we had another remicade infusion. So much is going on. I have been told four different things about this bacteria. The latest is it could have come from our family dog? He now is on what they called triple therapy. Amoxicillan, something thats starts with a C and another tummy protector. Heart Attack any one?
We were discharged Monday with no picc line. Celebrate, for sure. Nervous, definitely. He continues to do well. I am so knotted up about everything I can barely breathe. Today, we had another remicade infusion. So much is going on. I have been told four different things about this bacteria. The latest is it could have come from our family dog? He now is on what they called triple therapy. Amoxicillan, something thats starts with a C and another tummy protector. Heart Attack any one?
Saturday, March 31, 2012
This is going to be one long post....
So our IVIG, Cytoxan, and Remicade infusions went well. Sunday we were discharged. We loved our nurse. We were sent home on a G1 diet until he started tolerating a full diet with no diarrhea.
Monday Morning
Monday morning Gary had a well child check up scheduled. I thought why not. Kindergarden round up was Thursday so it would give me the perfect opportunity to chat with him about what to do. I had or do I have no intention of any kind of immunizations at this point. So the whole point became a complete act of God. As if He knew. I woke Gary up for a shower. He had crawled into bed with me at about 230 am with a temp of 102.0. Thought nothing of it because he has been running fevers. It aggrevated me because as a mother, you know. You know something. But tylenol and by morning as was ok. I dressed him. Gave him his medications. Put him in the car. He was quiet on the way. Too quiet. He moved very little. Asked very little questions. Not Gary. Gary is usually full of anxiety. He is about planning his day and what comes next to benefit him. What five year old isn't? Check in at the pediatrician, blood nose. Ok. No biggie. Odd to me but whatever, kids get bloody noses. Weight check, bp check, temp check. 101.4 Clearly not feeling well. He shook from the high fever. Our awesome pediatrician look him over. We talked about him not being ready especially being in the middle of new medications. On the table Gary looked awful. Our pediatrician asked questions. Asked if he had vomited. I said no. He said take him home, let him ride out the side effects of the chemotherapy. Ok. Pure honestly. The moment I scoped him up, I scrambled for my phone calling Children's Hospital as I walked out the door. Maybe I should have shown my pediatrician the respect of letting him know I was not comfortable with any of this. Only ten minutes into the car ride, he vomited. I was on my way to the Emergency Room at Children's. There was a little blood in the vomit but I though oh, bloody nose.
In the ER he was running a fever. They put him right back in the room. The rheumatologist showed up a lot quicker than normal. Gary was very sick. He acted funny with his movement. They felt confidant it was a reaction the IVIG infusion he recieved over the weekend. A harmless, well, bothersome, but nothing they could do anything for condition that would have to resolve on its own. Aspectic Menigitis. So benadryl and tylenol were given by mouth because we figured we were going home. Until his labs came back.
The two of many doctors that had chatted with me entered the room with a copy of the labs. The news was broke. My sister and her husband were sitting at my sides. It became a roller coaster ride. The works spinal tap spilled for her mouth like black sludge. My outter tough shell shattered into a million pieces, allowing the tears to instantly spill from my eyes. A lumbar puncture. I wanted to run. I wanted to leave. There was no oxgyen. But I had a job to do. I called my husband over facetime. "We just got some bad news." I explained he about the labs are elevated, like his white cell count was at 31,000. Inflammation markers and one in particular that called for the spinal tap, were all elevated. I cried. But I knew it was game time. I knew in an emergency room there is little time to prepare.
What seemed like a whole lot of people dressed into contamination gear filed in. It was very overwhelming. Doctors, nurses, and the four of us made for one full room. Gary cried in fear. He begged us to tell him what was going on. I couldn't. I didn't know what to say. Oh, your about to have a very large need poked deep inside your back. Yeah, not good to tell a five year old. Thank heavens for my sister. She remained almost stoic. So still, so calm, because she had too. She looked at Gary and said he was having a test done and everything would be ok. I could only weep. I could not look at him without fear. I was not helping. The sedative they were trying to give him through yet another IV, was not kicking in. A lot people standing around in the room, waiting for this five year old who comically enough would not shut up. The senior doc in charge of the procedure said until he is not making sense we need to keep pushing sedation. Three vails later at his max, it was go time. The annoucement of what was about to happen was chilling. "We are here with Gary Richard birthday. We will be preforming a lumbar puncture". Ok why don't you just sock me square in the nose while you say it. Maybe a quick knee in the stomach. We began to hold him. You can only image how important it is to keep a five year old still during something like this. Of course he was panicking. Hot, screaming, panicking. We had an oxgyen mask on his face to help him feel like he wasn't.
When I was a kid, we would love to rough house and put our siblings knees up to there chest and lay on top of them. I would often feel like you couldn't breathe. I can only venture to guess that is the way he felt. 5 adults had him. It wasn't working. The doctor who seemed in charge knocked the nurses out of the way. He said he had it. He pick Gary up, bent him in half with force, opening his spine. Gary was in misery. The man was shaking from muscle fatigue trying to keep him in place. It was pure choas. I was of course by his face, at the head of the bed, so I had full view of the procedure. The doctor performing the puncture shook. The large need shook. It was very difficult. So many things moving, yet this need to be done. It really did. Bacteria meningitis is something they can't miss. The needle finally went in. It was awful. It was just bad. They filled five tubes with his spinal fluid. After it was all said and done, the sedation took full effect. The room emptied, and he sucked on his "fresh air" high as kite. He was calm, tired, laying flat. They immediately began running antibiotics. There was no time for results.
That night, once we got up into our room, he was still sick. He ran high fevers all night. He sleep a little. He placed his hands behind his head and just layed there. The next morning he seemed better. The fevers however were still low grade hanging out. The next morning he felt better. His labs improved so much. The discharged with a diagnosis of a reaction to IVIG. No more IVIG. They were a little hestitant but confidant. So Wednesday afternoon we arrived home and he was doing fabulous. He ate dinner. Slept well. No worries. Thursday morning I got a call. I know Children's number and was expecting it to be the scheduler because I had just called her to check what was scheduled. I could hardly believe the words the rheumatology fellow spoke. He had a late growing lab come up positive. Please return to the ER. I floated, looking around my house as I spoke to him, "You are playing a joke on me, he is just fine." The voice replied it would never joke about something this serious.
I ripped my clothes off and started making calls in the shower. I called my husband, then my sisters. I called my Mom. My sister backed her bag back up and came over. I had no clean laundry. No food. No gas. We had just spent five days there. I was not prepared. I knew I had to go so I did a lot of pacing around my house. Gary was feeling fine at this point, which made it all that more difficult to go back. I stalled. I was afraid to tell Gary but since the antibiotics they ran on Monday, this kid is new. He is happy. He is euphoric. Part of me is nervous he is too happy. Like is this effecting his brain. We did it though. We packed up. Made a stop at his sisters school. I wanted to explain to her face to face what was going on. She cried. But there was nothing I could do. I had to go. I had to leave her there crying. Tears won over a blood infection in her brother. We came into the ER. They expected us. I promptly asked what the labs looked like. The intake nurse immediately looked it up. He tested positive in his urine and blood for a gramm rod negative bacteria. At the time he identified it as ecoli. A ecoli infection of the blood. Everyone was surprised how well he was doing despite what his labs were doing. I promptly reminded everyone that he had already recieved 48 hours worth of antibiotics. They were clearly already doing there job. But with a patient who is immune supressed, we are in dangerous territory. He had an xray done of his tummy. It was and still is the focus of the culpret of this bacteria. Weeks ago when Gary had the colonscopy done, they saw ulcers. I have a feeling it is not what they saw, but what they didn't see. The Xray however didn't show any preforations or abcesses. The more anitbiotic they give this child, the more super power he seems to have.
I wish I had more opportunity to update this, I will tell more later. We are so tired.
Monday Morning
Monday morning Gary had a well child check up scheduled. I thought why not. Kindergarden round up was Thursday so it would give me the perfect opportunity to chat with him about what to do. I had or do I have no intention of any kind of immunizations at this point. So the whole point became a complete act of God. As if He knew. I woke Gary up for a shower. He had crawled into bed with me at about 230 am with a temp of 102.0. Thought nothing of it because he has been running fevers. It aggrevated me because as a mother, you know. You know something. But tylenol and by morning as was ok. I dressed him. Gave him his medications. Put him in the car. He was quiet on the way. Too quiet. He moved very little. Asked very little questions. Not Gary. Gary is usually full of anxiety. He is about planning his day and what comes next to benefit him. What five year old isn't? Check in at the pediatrician, blood nose. Ok. No biggie. Odd to me but whatever, kids get bloody noses. Weight check, bp check, temp check. 101.4 Clearly not feeling well. He shook from the high fever. Our awesome pediatrician look him over. We talked about him not being ready especially being in the middle of new medications. On the table Gary looked awful. Our pediatrician asked questions. Asked if he had vomited. I said no. He said take him home, let him ride out the side effects of the chemotherapy. Ok. Pure honestly. The moment I scoped him up, I scrambled for my phone calling Children's Hospital as I walked out the door. Maybe I should have shown my pediatrician the respect of letting him know I was not comfortable with any of this. Only ten minutes into the car ride, he vomited. I was on my way to the Emergency Room at Children's. There was a little blood in the vomit but I though oh, bloody nose.
In the ER he was running a fever. They put him right back in the room. The rheumatologist showed up a lot quicker than normal. Gary was very sick. He acted funny with his movement. They felt confidant it was a reaction the IVIG infusion he recieved over the weekend. A harmless, well, bothersome, but nothing they could do anything for condition that would have to resolve on its own. Aspectic Menigitis. So benadryl and tylenol were given by mouth because we figured we were going home. Until his labs came back.
The two of many doctors that had chatted with me entered the room with a copy of the labs. The news was broke. My sister and her husband were sitting at my sides. It became a roller coaster ride. The works spinal tap spilled for her mouth like black sludge. My outter tough shell shattered into a million pieces, allowing the tears to instantly spill from my eyes. A lumbar puncture. I wanted to run. I wanted to leave. There was no oxgyen. But I had a job to do. I called my husband over facetime. "We just got some bad news." I explained he about the labs are elevated, like his white cell count was at 31,000. Inflammation markers and one in particular that called for the spinal tap, were all elevated. I cried. But I knew it was game time. I knew in an emergency room there is little time to prepare.
What seemed like a whole lot of people dressed into contamination gear filed in. It was very overwhelming. Doctors, nurses, and the four of us made for one full room. Gary cried in fear. He begged us to tell him what was going on. I couldn't. I didn't know what to say. Oh, your about to have a very large need poked deep inside your back. Yeah, not good to tell a five year old. Thank heavens for my sister. She remained almost stoic. So still, so calm, because she had too. She looked at Gary and said he was having a test done and everything would be ok. I could only weep. I could not look at him without fear. I was not helping. The sedative they were trying to give him through yet another IV, was not kicking in. A lot people standing around in the room, waiting for this five year old who comically enough would not shut up. The senior doc in charge of the procedure said until he is not making sense we need to keep pushing sedation. Three vails later at his max, it was go time. The annoucement of what was about to happen was chilling. "We are here with Gary Richard birthday. We will be preforming a lumbar puncture". Ok why don't you just sock me square in the nose while you say it. Maybe a quick knee in the stomach. We began to hold him. You can only image how important it is to keep a five year old still during something like this. Of course he was panicking. Hot, screaming, panicking. We had an oxgyen mask on his face to help him feel like he wasn't.
When I was a kid, we would love to rough house and put our siblings knees up to there chest and lay on top of them. I would often feel like you couldn't breathe. I can only venture to guess that is the way he felt. 5 adults had him. It wasn't working. The doctor who seemed in charge knocked the nurses out of the way. He said he had it. He pick Gary up, bent him in half with force, opening his spine. Gary was in misery. The man was shaking from muscle fatigue trying to keep him in place. It was pure choas. I was of course by his face, at the head of the bed, so I had full view of the procedure. The doctor performing the puncture shook. The large need shook. It was very difficult. So many things moving, yet this need to be done. It really did. Bacteria meningitis is something they can't miss. The needle finally went in. It was awful. It was just bad. They filled five tubes with his spinal fluid. After it was all said and done, the sedation took full effect. The room emptied, and he sucked on his "fresh air" high as kite. He was calm, tired, laying flat. They immediately began running antibiotics. There was no time for results.
That night, once we got up into our room, he was still sick. He ran high fevers all night. He sleep a little. He placed his hands behind his head and just layed there. The next morning he seemed better. The fevers however were still low grade hanging out. The next morning he felt better. His labs improved so much. The discharged with a diagnosis of a reaction to IVIG. No more IVIG. They were a little hestitant but confidant. So Wednesday afternoon we arrived home and he was doing fabulous. He ate dinner. Slept well. No worries. Thursday morning I got a call. I know Children's number and was expecting it to be the scheduler because I had just called her to check what was scheduled. I could hardly believe the words the rheumatology fellow spoke. He had a late growing lab come up positive. Please return to the ER. I floated, looking around my house as I spoke to him, "You are playing a joke on me, he is just fine." The voice replied it would never joke about something this serious.
I ripped my clothes off and started making calls in the shower. I called my husband, then my sisters. I called my Mom. My sister backed her bag back up and came over. I had no clean laundry. No food. No gas. We had just spent five days there. I was not prepared. I knew I had to go so I did a lot of pacing around my house. Gary was feeling fine at this point, which made it all that more difficult to go back. I stalled. I was afraid to tell Gary but since the antibiotics they ran on Monday, this kid is new. He is happy. He is euphoric. Part of me is nervous he is too happy. Like is this effecting his brain. We did it though. We packed up. Made a stop at his sisters school. I wanted to explain to her face to face what was going on. She cried. But there was nothing I could do. I had to go. I had to leave her there crying. Tears won over a blood infection in her brother. We came into the ER. They expected us. I promptly asked what the labs looked like. The intake nurse immediately looked it up. He tested positive in his urine and blood for a gramm rod negative bacteria. At the time he identified it as ecoli. A ecoli infection of the blood. Everyone was surprised how well he was doing despite what his labs were doing. I promptly reminded everyone that he had already recieved 48 hours worth of antibiotics. They were clearly already doing there job. But with a patient who is immune supressed, we are in dangerous territory. He had an xray done of his tummy. It was and still is the focus of the culpret of this bacteria. Weeks ago when Gary had the colonscopy done, they saw ulcers. I have a feeling it is not what they saw, but what they didn't see. The Xray however didn't show any preforations or abcesses. The more anitbiotic they give this child, the more super power he seems to have.
I wish I had more opportunity to update this, I will tell more later. We are so tired.
Saturday, March 24, 2012
Cytoxan, Rituxan, Remicade
Gary turned five years old on Wednesday. I knew on Tuesday he needed to come in. I knew after they did not admit us during the ER visit, that we were living on borrow time. I called and asked we spend his birthday at home. No one ever called back so I took that as a yes. By Thursday, the diarrhea was still getting worse. I made the call. They had us come in on Friday for a clinic and planned to be admitted.
It was good timing because on Thursday night, he ran a low grade fever, again. We got to meet our new doctor in clinic. She did a question and answer session, and catch up. She could see he was miserable. He needed to go to the bathroom a few times during the clinic visit. She said I am glad you brought him back in. He needs to be here.
Things happen quickly. I will have to get use to her new style. I like her aggressive approach. Right from the start of getting this whole thing put back on a different track, we stopped tacrolimus. So far that is a total of Cell Cept, Tacrolimus, and Enbrel. The plan was to admit him for a Remicade infusion. Remicade is used to treat IBD and JDM, so like I posted on the JM Mom's Board, it suddenly became a might as well, we need to do something. Of course they put him on Nothing by Mouth. I told them please don't do that. Run a high dose of steroids then don't let him eat. We got water, broth, and a popsicle. This morning he was up graded to a GI Limited diet. Mash potatoes, crackers, Pediasure, banana's, rice. Oddly, once given the clearance to eat he only had a graham cracker and the Chocolate Pediasure. The chocolate pediasure filled his tummy I think. I let the nurse know however, within 20 minutes he went 4 times. She didn't seem concerned so. He has been sleeping a lot. He slept 14 hours, and is napping now.
The plan now is to run Cytoxan and IVIG. We should be able to get out tomorrow. Then come back in two weeks for Rituxan and Pamidronate. Our pamidronate infusions she moved to once a month. Cytoxan will be once a month. Remicade will be in another two weeks, then 4, then move to 8. She does not know how long to run the Remicade. She has been communicating with one of the doctors that came back in June. They recommended the Enbrel shots which we noted no marked improvement or difference. So they think starting Cytoxan again is a good idea with the Rituxan.
This is all a lot.
This will be hard to take him home. Not knowing.
Gary's veins are irritated by all these infusions. He screams when saline is flushed through. We always stop to make sure his IV hasn't blown. But it is just that his body is irritated. How do I let them keep giving him all this stuff. I see pink eyelids. I see it. I see the JDM troll in the back of the dark woods rolling on the ground laughing and celebrating with evil. Well I am standing at the edge of those woods. Coming to get him with a baseball bat in hand. A beating is in order. That is how.
Thank you Summer for your note : ) I know you asked a few questions, I don't have the note you posted in front of me to answer.
It was good timing because on Thursday night, he ran a low grade fever, again. We got to meet our new doctor in clinic. She did a question and answer session, and catch up. She could see he was miserable. He needed to go to the bathroom a few times during the clinic visit. She said I am glad you brought him back in. He needs to be here.
Things happen quickly. I will have to get use to her new style. I like her aggressive approach. Right from the start of getting this whole thing put back on a different track, we stopped tacrolimus. So far that is a total of Cell Cept, Tacrolimus, and Enbrel. The plan was to admit him for a Remicade infusion. Remicade is used to treat IBD and JDM, so like I posted on the JM Mom's Board, it suddenly became a might as well, we need to do something. Of course they put him on Nothing by Mouth. I told them please don't do that. Run a high dose of steroids then don't let him eat. We got water, broth, and a popsicle. This morning he was up graded to a GI Limited diet. Mash potatoes, crackers, Pediasure, banana's, rice. Oddly, once given the clearance to eat he only had a graham cracker and the Chocolate Pediasure. The chocolate pediasure filled his tummy I think. I let the nurse know however, within 20 minutes he went 4 times. She didn't seem concerned so. He has been sleeping a lot. He slept 14 hours, and is napping now.
The plan now is to run Cytoxan and IVIG. We should be able to get out tomorrow. Then come back in two weeks for Rituxan and Pamidronate. Our pamidronate infusions she moved to once a month. Cytoxan will be once a month. Remicade will be in another two weeks, then 4, then move to 8. She does not know how long to run the Remicade. She has been communicating with one of the doctors that came back in June. They recommended the Enbrel shots which we noted no marked improvement or difference. So they think starting Cytoxan again is a good idea with the Rituxan.
This is all a lot.
This will be hard to take him home. Not knowing.
Gary's veins are irritated by all these infusions. He screams when saline is flushed through. We always stop to make sure his IV hasn't blown. But it is just that his body is irritated. How do I let them keep giving him all this stuff. I see pink eyelids. I see it. I see the JDM troll in the back of the dark woods rolling on the ground laughing and celebrating with evil. Well I am standing at the edge of those woods. Coming to get him with a baseball bat in hand. A beating is in order. That is how.
Thank you Summer for your note : ) I know you asked a few questions, I don't have the note you posted in front of me to answer.
Monday, March 19, 2012
Update
Gary is doing good. After a visit to the ER last week for a fever that wouldn't break on Wednesday, he seems to be bouncing back.
101.4, 102.2 even with tylenol, we called to see what they wanted us to do. The kids were just arriving home from school when we packed up. Elexis was just as upset as Gary was about having to leave. Elexis was turning ten the next day. I couldn't tell her whether or not we would be returning home. We can only be twoo careful however. The hospital is dreaded. I am sure it is for most people. However, when the effect of distraction because something outbod your routine is happening that tends to distract you. When you have been doing this for three years, that whole concept only plunges you into the unpleasantness of the ER visit. Gary wasn't sick per say. It was just the pesky fever that kept going up despite treating it. An emergency room isn't the best place for an immune suppressed kid to be but we had to do what we had to do. Not sure that is playing it entirely safe especially since it was like a scene from The Walking Dead (a tv show a few members of my family watch that I can't because it is too intense, zombies, blah). When they finally got us back to room, the rheumatologists intern who had just seen us from the week before popped in to say hello. She was on her way out for the day. We talked about what was going on. She said they were talking about admitting us, and getting the medications going that we were waiting on starting until he recovered. After an IV start, and one nasal swab later, labs looked so much better than they did the week before. The 5ml of steroids are bringing those labs down nicely. Not to mention it is also knocking out the heliotrope rash. Inflammation markers are still very elevated, a few started to trend down. The ER doctors came in, went through the usual student doctors. A mirage of questions, me educating them on what they are dealing with. Pleasantly, the student doctor knew of JDM, and DM as well. His neighbor, while growing up had JDM, and so did the father of this child. I always thought that was very rare but it is said to be genetic. The father I am familiar with. I remember reading about him. He was a famous football player in the seventies. Suddenly he became very tired. Running the football field became a huge challenge for him, ending his career. Anyway, another lab came back from the nasal swab. It tested positive for a virus, the coronavirus. Basically it is the common cold virus that is respiratoryish. It can cause many things. They asked if we wanted to go home since we knew what was causing this fever. I wish that made things easy. I knew getting that diagnosis was my chance to escape. There is nothing they can do for a virus but with a child who has what he has and its all complicated, you would think they would want to keep an eye on things. The rheumatologist who was attending did not even bother to come talk to us. They got the go ahead to release us. Our whole ER ordeal took about seven hours. We had spent enough time in the hot zone. I was feeling like the best thing to do was to get the heck out of there before we picked up something else. After sharing a bathroom with a little girl who looked terrible and another kid who practically puked at our feet, yeah, done. Gary was in the bathroom about ten times. I had no choice but to run out of there. My favorite part of the ER was by the time we got there, the fever broke. Ugghhh!
The next morning I called rheumatology to see if I was suppose to hold the methotrexate shot because of the virus. They called back and said yes. Later that day one of our doctors called to say we were suppose to be admitted. The wanted to get to work on stopping the diarrhea that had returned. Somehow, the ER didn't get the message. Neither did the rheumatologist on call. Everything happens for a reason.
One of the plans after the Thursday meeting is to bring us in. In order to give Gary immediate rest and healing to his colon, they want to check him in and put him on TPN, while on NPM. That means for a few days he wont be allowed to eat, and given nutrition by Iv. Uh, no. They want to start remicade which I am comfortable with of course but not the whole TPN thing. We have been on that before and it is difficult. Very difficult. I mean, I only will approve this if he just doesn't get better and it is completely necessary. I asked her to give me a few more days. i told her want this virus to cycle outbofbour house. Yep, we all ended up getting sick. Sneezing, congestion, nose burning, ect,. Give him a little more time to improve. Let the steroids keep working. The flare has come under control. He stopped having blood in his diarrhea. Let's just see. If I don't like what is going on, then I will bring him him. She was completely agreed. She said they are willing to let me drive this.
Where is the car headed? Well, he seems to have had a good day yesterday. The day before he did go 17 times. It wasn't all diarrhea but he still has one set of active bowels. The next day he went 8 times so big improving. I still am getting the feeling we are living on borrowed time however. I had hoped to make it too our original appointment on the 27th. On Wednesday he turns 5. No birthday in one of his least favorite places. We will see by the end of the week.
101.4, 102.2 even with tylenol, we called to see what they wanted us to do. The kids were just arriving home from school when we packed up. Elexis was just as upset as Gary was about having to leave. Elexis was turning ten the next day. I couldn't tell her whether or not we would be returning home. We can only be twoo careful however. The hospital is dreaded. I am sure it is for most people. However, when the effect of distraction because something outbod your routine is happening that tends to distract you. When you have been doing this for three years, that whole concept only plunges you into the unpleasantness of the ER visit. Gary wasn't sick per say. It was just the pesky fever that kept going up despite treating it. An emergency room isn't the best place for an immune suppressed kid to be but we had to do what we had to do. Not sure that is playing it entirely safe especially since it was like a scene from The Walking Dead (a tv show a few members of my family watch that I can't because it is too intense, zombies, blah). When they finally got us back to room, the rheumatologists intern who had just seen us from the week before popped in to say hello. She was on her way out for the day. We talked about what was going on. She said they were talking about admitting us, and getting the medications going that we were waiting on starting until he recovered. After an IV start, and one nasal swab later, labs looked so much better than they did the week before. The 5ml of steroids are bringing those labs down nicely. Not to mention it is also knocking out the heliotrope rash. Inflammation markers are still very elevated, a few started to trend down. The ER doctors came in, went through the usual student doctors. A mirage of questions, me educating them on what they are dealing with. Pleasantly, the student doctor knew of JDM, and DM as well. His neighbor, while growing up had JDM, and so did the father of this child. I always thought that was very rare but it is said to be genetic. The father I am familiar with. I remember reading about him. He was a famous football player in the seventies. Suddenly he became very tired. Running the football field became a huge challenge for him, ending his career. Anyway, another lab came back from the nasal swab. It tested positive for a virus, the coronavirus. Basically it is the common cold virus that is respiratoryish. It can cause many things. They asked if we wanted to go home since we knew what was causing this fever. I wish that made things easy. I knew getting that diagnosis was my chance to escape. There is nothing they can do for a virus but with a child who has what he has and its all complicated, you would think they would want to keep an eye on things. The rheumatologist who was attending did not even bother to come talk to us. They got the go ahead to release us. Our whole ER ordeal took about seven hours. We had spent enough time in the hot zone. I was feeling like the best thing to do was to get the heck out of there before we picked up something else. After sharing a bathroom with a little girl who looked terrible and another kid who practically puked at our feet, yeah, done. Gary was in the bathroom about ten times. I had no choice but to run out of there. My favorite part of the ER was by the time we got there, the fever broke. Ugghhh!
The next morning I called rheumatology to see if I was suppose to hold the methotrexate shot because of the virus. They called back and said yes. Later that day one of our doctors called to say we were suppose to be admitted. The wanted to get to work on stopping the diarrhea that had returned. Somehow, the ER didn't get the message. Neither did the rheumatologist on call. Everything happens for a reason.
One of the plans after the Thursday meeting is to bring us in. In order to give Gary immediate rest and healing to his colon, they want to check him in and put him on TPN, while on NPM. That means for a few days he wont be allowed to eat, and given nutrition by Iv. Uh, no. They want to start remicade which I am comfortable with of course but not the whole TPN thing. We have been on that before and it is difficult. Very difficult. I mean, I only will approve this if he just doesn't get better and it is completely necessary. I asked her to give me a few more days. i told her want this virus to cycle outbofbour house. Yep, we all ended up getting sick. Sneezing, congestion, nose burning, ect,. Give him a little more time to improve. Let the steroids keep working. The flare has come under control. He stopped having blood in his diarrhea. Let's just see. If I don't like what is going on, then I will bring him him. She was completely agreed. She said they are willing to let me drive this.
Where is the car headed? Well, he seems to have had a good day yesterday. The day before he did go 17 times. It wasn't all diarrhea but he still has one set of active bowels. The next day he went 8 times so big improving. I still am getting the feeling we are living on borrowed time however. I had hoped to make it too our original appointment on the 27th. On Wednesday he turns 5. No birthday in one of his least favorite places. We will see by the end of the week.
Saturday, March 10, 2012
Where To Begin
I wish I could start this with telling you about our March infusion. I wish I could say it was all easy peasy. but it wasn't. Monday was our clinic appointment. We saw our rheumatologist for the last time in clinic. She is retiring in April. Everything at that point seemed fine. Gary had run low grade fevers three different times in February. We treated with tylenol and no other symptoms besides the obvious and same old diarehha. By Tuesday things took a turn. The fevers took a turn for the worse. He woke up at 8am. Came down stairs and went to back to bed on the couch till 1pm. I kept checking on him. I noticed his face swelling in his sleep, and a rash coming in. When he finally woke up, I gave him lunch. He ate a little bit then complained of headache. I found the tylenol and noticed he was warm. A fever of 102. Before the tylenol could digest he vomited explosively. I called and left a message with the nurse. I assumed they would tell me not to come in for his infusion the next day. But his doctor wanted him in. Fever or not. He felt much better after vomiting and even ate a little dinner that night and kept down his steroid dose. But at 10pm another fever. At this point I had a choice. Give him more tylenol and sleep one last night in my bed or head to the ER. We are veterans of this. We have been here before. So I decided to give him tylenol. If the fever broke then we would get up early and head to the hospital. If it didn't then we would head out at midnight. The fever broke. We slept the night, well barely for me anyway. The next morning we were admitted. Things started to unfold. During the clinic appointment it had been determined that Gary would need a colonscopy and endoscopy. A level of inflammation was detected in a stool sample. It was a level that was suppose to be 100 but came back to be 2500. With that they said it was worth investigating further. He was already scheduled to be admitted for IVIG and pamidronate so they were able to get him in for the colonscopy and endoscopy.
Scope
The endoscopy and colonscopy was really hard. After the labs came back crazy high, we got comfortable for an overnight. Something is not right. As soon as we checked in it was deteremined that he was scheduled so nothing by mouth was ordered. The day before he was vomiting so he was really thirsty. My day and his day went from bad to worse. After two hours of begging for something to drink, he was finally cleared for clears. Chicken broth, jello, sprite, or clear candy. All mixed with Miralax to clean him out for the colonscopy and endoscopy. On top of already having diarreha plus giving him benadryl and the IVIG. Made for an interesting time. Imagine being sleepy but need to go to the bathroom. He was miserable. The misery sent him into a breakdown. He awoke from a nap. He was mad. He kept standing on the side of his bed screaming, calling me names. He threatened to pull his IV out. He would not let the nurses touch him. They needed to get vitals. It was impossible. As we came towards the end of the IVIG he became even more agitated. Despite running it over a ten hour rate, stopping the infusion half way and giving him benadryl, he still had a reaction. A large headache, hives rash all over his chest and unnatural irritation. We abruptly stopped the IVIG. They tried to run more benadryl but he was very intolerant. I told them to turn off the IV, he had enough. He was suppose to get pamidronate after that but he clearly had enough. The IV was flushing fine but every time they tried to even push a flush, he responded. Everytime we turned it off, he fell aspleep. It was agreed to let him sleep through the night. He had a procedure in the morning. The day before he had been throwing up. His body had enough. He slept the night away. Well, in between vital checks at which point they detected irregular heartbeat. Turned out to be nothing. Then his Bp dropped too low. The nurses didn't like it but the doctors said it would be ok. For the most part, his BP is on the high end. So being too low was a nice change.
MOMMY I AM SCARED
We woke up the next morning at about 730. We were scheduled to be transported to the surgery center for the procedure at 9am. I was releaved when they came early. After midnight before he was under NOTHING BY MOUTH at all until after the procedure. So 8:15 rolled around and they came and got us. Thank you Lord. The quicker they got him in the better. I had not taken the time to tell him what was about to happen. I didn't know how. How do you make a five year old understand? I decided to wait until we were in the prep room. I explained they were going to give him medicine to make him sleepy. He was going to take a nap. The bad IV from the night before was removed before so I was thankful to hear they were going gas him before starting a new IV. He cried. He cried a lot. He told me he was scared. Several times he needed to use the bathroom. It was hard to talk to nurses and doctors in between running him to the bathroom. He broke my heart with begging me, "Mommie, please. I scared. I soo scared. Don't let them put me to sleep." He cried for his Aunt and Uncle. Thank the Lord again to them for coming again! It made it easier. It was time to wheel him into the procedure room. He wept. He wept as they placed the gas mask over his face. I stayed as close as I could to him. I remained positive and non chalant so he would not be scared. I acted as if it was no big deal. I refused to take my game face off. As the gas took affect, his eyes rolled into the back of his head. His knees fell to the outside of his body and he was quickly asleep. The doctors looked at me and said, "ok Mom, give him a kiss". I blew a kiss, he was out of my reach. I couldn't bring myself to actually place my lips on his skin for fear the tears would flow in front of them. I was not going to let that happen. Game face. Quickly out the doors with my sister and my brother in law. I marched. I marched straight faced. I found a chair, sat, and barried my face in my hands, letting my emotions flow. I kept it to five minutes. After my sister said something to make me laugh, we went for coffee. An hour later, we got the page to return to the procedure doors to meet the doctor.
RESULTS
The results of the scopes did find he has ulcerations in his colon. Blood in the diarreha makes sense now. It is why that is on hold. Throat and stomach look normal. The ulcerations in his colon are on the deep side but not crazy. They took biospies. They also took a lot of blood to test everything. They want to make sure we are covering everything. Infections, bacteria, viruses, ect,.
RECOVERY
After we talked to the doctor he told us he was back in his room. We bolted across the hospital to get over to the room. He wasn't there. He was still in recovery. We were told to wait in the room. I couldn't. I couldn't sit there while my child woke up after begging not to put him to sleep. I had to be there. The nurse sent us back to where we were. It was hard getting back there into the procedure room. They would not let me back there until he was waking up. They put me in a room the was for people going into procedures. I sat alone for 45 minutes. Finally there he was. Crying in recovery. Not much but he survived! : ) We didn't spend much time in there and got back to our room. Back in his room he slept. He didn't even bother to eat. He just slept. I decided that we would come back for the other infusion we skipped the night before. He had been through enough. I had enough and so did he. The doctors were fine with that. We wanted to wait for him to wake up to make sure he was eating and going to the bathroom. He woke up in a good mood and immediately started eating and drinking.
HOME, Not HOME
We started packing up because there was no use sitting around waiting for test results. We noticed Gary's face was pretty swollen while slept in recovery. When he woke, the infamous JDM rash set in hard. His eyes were purple pink, and his lips were huge. I was concerned put thought it was from the fact he had a breathing tube down in throat. That maybe that trauma was contributing. We were packing bags, and getting ready to get out of there when the nurse said, "the phone is about to ring, please pick it up, its the doctor." She explained that they had done tested his blood for levels of his medications. One lab was in, the cell cept or MMF. It read 0. It meant that he is not absorbing his medications. She asked us to hang out a little longer until they could talk, and figure things out. The bright pink eye shadow he was wearing suddenly started making sense. High labs, bright JDM rash, vomiting, he is flaring. An hour later, after I stopped spinning they came in. I immediately told them he needed to be pulsed with steroids. I told them I felt his JDM is flaring. He is no longer on cellcept. They also discontinued the enbrel shots. Deciding to pull him off of what we can right now is better. The next morning we were going to determine what to do next. Since tests weren't going to be in till next week, they upped his steroid dose back up to 5ml. From 1ml to 5ml. After the intravenous pulse he looked a little better. We had opted to skip his methotrexate shot the night before because at the time we thought he was "sick". It is looking less and less like that is what is happening. That it is in fact, JDM. Since we were working on our third day in the hospital, we went ahead and did our pamidronate infusion.
So now we wait for Monday, possibly Tuesday. He is doing better but everything is in the air. I hate hanging.Our nurse flushing his iv in his foot. She was awesome!
Scope
The endoscopy and colonscopy was really hard. After the labs came back crazy high, we got comfortable for an overnight. Something is not right. As soon as we checked in it was deteremined that he was scheduled so nothing by mouth was ordered. The day before he was vomiting so he was really thirsty. My day and his day went from bad to worse. After two hours of begging for something to drink, he was finally cleared for clears. Chicken broth, jello, sprite, or clear candy. All mixed with Miralax to clean him out for the colonscopy and endoscopy. On top of already having diarreha plus giving him benadryl and the IVIG. Made for an interesting time. Imagine being sleepy but need to go to the bathroom. He was miserable. The misery sent him into a breakdown. He awoke from a nap. He was mad. He kept standing on the side of his bed screaming, calling me names. He threatened to pull his IV out. He would not let the nurses touch him. They needed to get vitals. It was impossible. As we came towards the end of the IVIG he became even more agitated. Despite running it over a ten hour rate, stopping the infusion half way and giving him benadryl, he still had a reaction. A large headache, hives rash all over his chest and unnatural irritation. We abruptly stopped the IVIG. They tried to run more benadryl but he was very intolerant. I told them to turn off the IV, he had enough. He was suppose to get pamidronate after that but he clearly had enough. The IV was flushing fine but every time they tried to even push a flush, he responded. Everytime we turned it off, he fell aspleep. It was agreed to let him sleep through the night. He had a procedure in the morning. The day before he had been throwing up. His body had enough. He slept the night away. Well, in between vital checks at which point they detected irregular heartbeat. Turned out to be nothing. Then his Bp dropped too low. The nurses didn't like it but the doctors said it would be ok. For the most part, his BP is on the high end. So being too low was a nice change.
MOMMY I AM SCARED
We woke up the next morning at about 730. We were scheduled to be transported to the surgery center for the procedure at 9am. I was releaved when they came early. After midnight before he was under NOTHING BY MOUTH at all until after the procedure. So 8:15 rolled around and they came and got us. Thank you Lord. The quicker they got him in the better. I had not taken the time to tell him what was about to happen. I didn't know how. How do you make a five year old understand? I decided to wait until we were in the prep room. I explained they were going to give him medicine to make him sleepy. He was going to take a nap. The bad IV from the night before was removed before so I was thankful to hear they were going gas him before starting a new IV. He cried. He cried a lot. He told me he was scared. Several times he needed to use the bathroom. It was hard to talk to nurses and doctors in between running him to the bathroom. He broke my heart with begging me, "Mommie, please. I scared. I soo scared. Don't let them put me to sleep." He cried for his Aunt and Uncle. Thank the Lord again to them for coming again! It made it easier. It was time to wheel him into the procedure room. He wept. He wept as they placed the gas mask over his face. I stayed as close as I could to him. I remained positive and non chalant so he would not be scared. I acted as if it was no big deal. I refused to take my game face off. As the gas took affect, his eyes rolled into the back of his head. His knees fell to the outside of his body and he was quickly asleep. The doctors looked at me and said, "ok Mom, give him a kiss". I blew a kiss, he was out of my reach. I couldn't bring myself to actually place my lips on his skin for fear the tears would flow in front of them. I was not going to let that happen. Game face. Quickly out the doors with my sister and my brother in law. I marched. I marched straight faced. I found a chair, sat, and barried my face in my hands, letting my emotions flow. I kept it to five minutes. After my sister said something to make me laugh, we went for coffee. An hour later, we got the page to return to the procedure doors to meet the doctor.
RESULTS
The results of the scopes did find he has ulcerations in his colon. Blood in the diarreha makes sense now. It is why that is on hold. Throat and stomach look normal. The ulcerations in his colon are on the deep side but not crazy. They took biospies. They also took a lot of blood to test everything. They want to make sure we are covering everything. Infections, bacteria, viruses, ect,.
RECOVERY
After we talked to the doctor he told us he was back in his room. We bolted across the hospital to get over to the room. He wasn't there. He was still in recovery. We were told to wait in the room. I couldn't. I couldn't sit there while my child woke up after begging not to put him to sleep. I had to be there. The nurse sent us back to where we were. It was hard getting back there into the procedure room. They would not let me back there until he was waking up. They put me in a room the was for people going into procedures. I sat alone for 45 minutes. Finally there he was. Crying in recovery. Not much but he survived! : ) We didn't spend much time in there and got back to our room. Back in his room he slept. He didn't even bother to eat. He just slept. I decided that we would come back for the other infusion we skipped the night before. He had been through enough. I had enough and so did he. The doctors were fine with that. We wanted to wait for him to wake up to make sure he was eating and going to the bathroom. He woke up in a good mood and immediately started eating and drinking.
HOME, Not HOME
We started packing up because there was no use sitting around waiting for test results. We noticed Gary's face was pretty swollen while slept in recovery. When he woke, the infamous JDM rash set in hard. His eyes were purple pink, and his lips were huge. I was concerned put thought it was from the fact he had a breathing tube down in throat. That maybe that trauma was contributing. We were packing bags, and getting ready to get out of there when the nurse said, "the phone is about to ring, please pick it up, its the doctor." She explained that they had done tested his blood for levels of his medications. One lab was in, the cell cept or MMF. It read 0. It meant that he is not absorbing his medications. She asked us to hang out a little longer until they could talk, and figure things out. The bright pink eye shadow he was wearing suddenly started making sense. High labs, bright JDM rash, vomiting, he is flaring. An hour later, after I stopped spinning they came in. I immediately told them he needed to be pulsed with steroids. I told them I felt his JDM is flaring. He is no longer on cellcept. They also discontinued the enbrel shots. Deciding to pull him off of what we can right now is better. The next morning we were going to determine what to do next. Since tests weren't going to be in till next week, they upped his steroid dose back up to 5ml. From 1ml to 5ml. After the intravenous pulse he looked a little better. We had opted to skip his methotrexate shot the night before because at the time we thought he was "sick". It is looking less and less like that is what is happening. That it is in fact, JDM. Since we were working on our third day in the hospital, we went ahead and did our pamidronate infusion.
So now we wait for Monday, possibly Tuesday. He is doing better but everything is in the air. I hate hanging.Our nurse flushing his iv in his foot. She was awesome!
Tuesday, February 21, 2012
Lots of things going on
So it seems Gary may have picked up a little virus last week. Valentines evening he ran a fever suddenly. I gave him tylenol and his fever was better. With the diarrhea Gary already had, adding a stomach virus on top of it made for a lot of bathroom trips. A lot. Diarrhea has been in our news for quite awhile. We even saw a G. I. Specialist to see if further testing needed to be done, to see if it was the medications, or what was going on. At this appointment we also talked about his cough. The cough has eased up but really its a cruel joke to have a cough and diarrhea at the same time. Something has to be fixed. We did some lab testing to make sure there were no bacteria's growing inside him or anything like that. Funny after the appointment he came down with something. Last week he did not receive his methotrexate shot or enbrel. It was a little tough for me because the next day on the 15th he ran a low grade fever. The clinic was busy and our doctor was on call so it took them more than 3 hours to get back to me. I wasn't panicked for my own sanity I wish they could have called sooner. But instincts are still intact. Besides he was still eating and drinking. Monday he came down with mouth sores again. Like normal things were HOT. I did see places in his mouth that looked like sores or something. So Monday, Presidents day they were not in. Ok fine! One more day but I was going insane. I was up at the crack of dawn this morning leaving long messages. They returned my call immediately. Our doctor couldn't see him today because the schedule was booked. So she had us run him up to our pediatrician. It was good to catch up with him. He is the one who thinks it is indeed a virus of some kind. He prescribed malox and benadryl for the mouth sores. What confuses me most is back in November when he flared, the inside of his mouth did the same thing. I do admit this does seem to be a bit different but still. We headed to Children's to do pick up some medicines. My phone rang as I pulled in. It was the GI clinic. Apparently the sample we gave a couple weeks ago didn't give what they needed. Just so happens, Yay! we were there to do it again. Then my phone rang again saying they were filling a prescription to slow down his colon. I am a bit nervous it will slow it down too much and we will have the opposite problem. I just want his tummy pain to stop. Tonight, after his first dose, we had success with diarrhea easing up but not the stomach pain so far. But its only been hours. Keeping a close eye. If this doesn't work they are talking about scope him from both ends or cutting back on medications. Both sound awful and scary.
I am going on vacation. My children are staying with my sister. Yes, this makes me even more nervous to leave for 5 days but the trip was a gift from my brother.
I am going on vacation. My children are staying with my sister. Yes, this makes me even more nervous to leave for 5 days but the trip was a gift from my brother.
Monday, February 13, 2012
February Infusion
Oh its always fun. Every infusion is different. I can giggle now. *Note to self: Never infuse in front of nurses station. They talk about a lot more than just medical stuff. Don't get me wrong, they were appropriate but even when they disagree with each other or other people, its not fun. The volume on my ipad wouldn't go loud enough. It's like taking a nap in the middle of a cocktail party.
Gary did good though. He was on the floor because their chairs are just not his size. I am going to bring a blow up mini mattress from now on. Next month we are admitted to the hospital because he gets IVIG and Pamidronate.
Gary's labs are doing fine still. He did have a lot L's on it this time that I am not use to seeing. I asked the nurse right why is almost all his numbers marked with a High or Low symbol. She started to go through each number and explained that with all his medications and the fact he has a disease that they expect that. She said his labs are very close to normal like by one number so it is nothing to worry about. Yeah. Ok.
We dealt with the drama of not having enough time in the infusion center. They came to me and said, "the infusion center closes at 730. At the rate we have his infusion set and the delay, we are going to run out of time so here is what we are going to do. I already called the doctor and she ok'd it. We are going to bump the rate of up at the end in order to get the entire treatment finished." She sat there and rambled on about how it was important he get the whole dose. Blah. Blah. Blah. I said no. I told her I don't feel comfortable risking making him sick or pushing a reaction because people are inconvenienced by time and want to go home. I told her I would be willing to come back tomorrow and go home with the IV in. We had an appointment with a GI specialist so whatever, no big deal. Then I said what about just admitting us then? Put us on the floor. She said they won't do that. Ok. Moments later our Doctor dropped in. She was checking on Gary. I told her I am not comfortable with pushing the rate of the infusion. She said no problem. We will just admit you. I looked at the nurse and said, "yeah, I asked about that". They were agitated. The nurse said we have to wait for admission to call when a bed is ready. Dr. E said there is no bed shortage that she had heard of so it shouldn't be a problem. After the doctor left I heard a small discussion about exceptions and the what not's of the whole situation. Left hand talking to the right hand. The nurse came back and said we probably wouldn't be admitted until 630. Well Gary is sleeping on the floor right now so why not just send us now so he can sleep in a bed. Get settle, get comfy, get away from all this noise. She said she didn't have control of that. She had to wait for admission to call her. Ok, because they knew that if we were admitted at 630 by the time admission was complete, we would be ready for discharge. So after all this 630 rolled around and in walked a charge nurse with a calculator and 2 other nurses. She figured out that we would indeed be finished by 730. Really, after all that. Made me giggle in a exhausted sort of way.
The Popsicle
After Gary awoke from his benadryl coma, he had hankering for a popsicle. They didn't have any. So for one of the first times in our history with Seattle Childrens Hospital, I left him alone. Awake. I have snuck down to Starbucks maybe once or twice. I ask the nurse to watch him as her desk was right in front of where we were being infused. It was quick and did the trick.
Gary did good though. He was on the floor because their chairs are just not his size. I am going to bring a blow up mini mattress from now on. Next month we are admitted to the hospital because he gets IVIG and Pamidronate.
Gary's labs are doing fine still. He did have a lot L's on it this time that I am not use to seeing. I asked the nurse right why is almost all his numbers marked with a High or Low symbol. She started to go through each number and explained that with all his medications and the fact he has a disease that they expect that. She said his labs are very close to normal like by one number so it is nothing to worry about. Yeah. Ok.
We dealt with the drama of not having enough time in the infusion center. They came to me and said, "the infusion center closes at 730. At the rate we have his infusion set and the delay, we are going to run out of time so here is what we are going to do. I already called the doctor and she ok'd it. We are going to bump the rate of up at the end in order to get the entire treatment finished." She sat there and rambled on about how it was important he get the whole dose. Blah. Blah. Blah. I said no. I told her I don't feel comfortable risking making him sick or pushing a reaction because people are inconvenienced by time and want to go home. I told her I would be willing to come back tomorrow and go home with the IV in. We had an appointment with a GI specialist so whatever, no big deal. Then I said what about just admitting us then? Put us on the floor. She said they won't do that. Ok. Moments later our Doctor dropped in. She was checking on Gary. I told her I am not comfortable with pushing the rate of the infusion. She said no problem. We will just admit you. I looked at the nurse and said, "yeah, I asked about that". They were agitated. The nurse said we have to wait for admission to call when a bed is ready. Dr. E said there is no bed shortage that she had heard of so it shouldn't be a problem. After the doctor left I heard a small discussion about exceptions and the what not's of the whole situation. Left hand talking to the right hand. The nurse came back and said we probably wouldn't be admitted until 630. Well Gary is sleeping on the floor right now so why not just send us now so he can sleep in a bed. Get settle, get comfy, get away from all this noise. She said she didn't have control of that. She had to wait for admission to call her. Ok, because they knew that if we were admitted at 630 by the time admission was complete, we would be ready for discharge. So after all this 630 rolled around and in walked a charge nurse with a calculator and 2 other nurses. She figured out that we would indeed be finished by 730. Really, after all that. Made me giggle in a exhausted sort of way.
The Popsicle
After Gary awoke from his benadryl coma, he had hankering for a popsicle. They didn't have any. So for one of the first times in our history with Seattle Childrens Hospital, I left him alone. Awake. I have snuck down to Starbucks maybe once or twice. I ask the nurse to watch him as her desk was right in front of where we were being infused. It was quick and did the trick.
Thursday, February 2, 2012
Poisen
Have you ever heard you have a choice how you deal with life? I believe there is truth to that. But I don't believe it is entirely 100% correct. I believe that everyone is different. Our bodies are different. Our chemicals are different. What seems like no big deal to someone else is so much more to someone else. I have dealt with this my entire life. The poison I call it. When something triggers me that I don't care for, I can feel it go through my body. Its like a leak of yuck in me, producing foul, anger, sad emotions. Over things I would normally shrug off. Over things I know will turn out fine. But no matter how many times I tell myself this fact, it still gets me, creeps back in. It kind of feels like depression or maybe grief. My grief yesterday was triggered at Gary's clinic appointment.
Rheumatologist Retirement
"Don't you look nice!" she said as she entered the room. I thanked her and thought what a nice compliment. We started with our usual chit chat. How are you? How is he? How are things? Long list, and she saved the best for last. I will get back to Gary later. "Erika, I have something to tell you". That triggered no emotion in me. It didn't strike me until the next sentence. "I'm retiring." She intently smiled and grimaced and waited. I don't go around asking woman how old they are. I couldn't believe I didn't realize it was time. She is 65. She has done her time. But my reaction. Panic. My thoughts spun. They pushed forward then swung back. I went into a stare. Then tears welled up, went away, and came back as I said, "you can't, you can't do this." As my emotions and ration kicked in I went into what a polite selfless person does and congratulated her. Told her I understood. I began to thank her, because that was in fact my heart, I am thankful. Then I stared some more. She told me I have done an excellent job in Gary's care. She was being sincere, but again, its a natural reaction to smooth it over. She stared at me. Another round of tears came and went. We reminded each other of past treatments, and what a wild ride it has been for Gary. I told her given the severity of Gary's case, that she and her team had done a very impressive job of getting him back and keeping him functioning. I suppose I am so upset with this because as a patient there is a vulnerability of connection. I connect all the bad news that has come with this disease, and the good. Even when I had complaints, there was always praise and gratefulness. I have been mad at her for silly things. But I can't barely remember those. I know it will be alright. I already called and am on the schedule to have another doctor with the same level of experience, whom I respect, take over. She told me I was on the list of patients she was most worried to tell. The emotions this triggers is unbelievable. I do tend to be emotionally dramatic maybe a bit irrational when I hear things I don't care for. Not loud or rude, well maybe but she was right to worry. I'm still trying to entirely connect I'm taking this so hard. I am in the market for a fabulous retirement gift. I know with time I will mend. LOL. Feel like I am going through a break up.
MY BOY
Before the bomb was lowered, we went through all the discussion. I told her I was done with this cough. I wanted it to stop. Please help me get this fixed. Same with the diarrhea he has 12 times a day. She is wonderful, she wants it fixed too. Tomorrow we have a CT of his sinuses to see if its a drain. If its not his sinuses then we will check if it is coming from his tummy. She said she would check with the GI department to see if we could prescribe an anti spasm medication for his colon. We moved on to JDM stuff. I told her his nail folds look like crap. She wrote down bad. She giggled and said, "I will write bad if thats ok?". She is very much use to me. Upon examining she said, "I don't know, they don't look". She stopped when she moved on to the next finger, and the next. Did a never mind. He has one or two fingers that are ok but the rest you can see visible dilation of the blood vessels. I let her know there are a few new calcium deposits in his face. The calcinosis around his tailbone is showing signs of surfacing. For a few days I thought they might be a little pimple or something. Most the time I can gently schratch something like that off. It didn't. She talked about seeing a surgeon so they are aware of him. However, upon examination she said they are pretty deep still so it could wait. We are under doctors orders to still gently. She did his strength test. We had a conversation about Gary's hesitation with stairs and certain things he can't do that leave me seeing muscle weakness. She made a remark about how strong he is after doing the test. I know she doesn't say that to negate what I am seeing or make me feel like a crazy Mom. The victory was mine however at our next appointment. Gary had a physical therapy evaluation.
PT
I can't wait till she gets the report on this one. The therapist hit every point I was seeing. His function his there but his strength is not there to support it. He has hip and leg weakness. He straightens his left leg. The therapist said it could be from calcium, "he goes up and down the stairs with a lot of compensation, like leaving his leg straight, pivoting his hip", much like an eighty year old man. I am not sure how many times a week we will be doing physical therapy yet, but the orders will be doing in. Time to get this boy strong or stronger.
SocCoR
Gary is such a sports guy. He loves it. So I signed him up for soccer. Hopefully he will just stand there and look cute so the ball doesn't hit him or anything like that. Doubt it. It will be good for him? Hands over eyes.
Infusion next week. Not looking forward to it.
Rheumatologist Retirement
"Don't you look nice!" she said as she entered the room. I thanked her and thought what a nice compliment. We started with our usual chit chat. How are you? How is he? How are things? Long list, and she saved the best for last. I will get back to Gary later. "Erika, I have something to tell you". That triggered no emotion in me. It didn't strike me until the next sentence. "I'm retiring." She intently smiled and grimaced and waited. I don't go around asking woman how old they are. I couldn't believe I didn't realize it was time. She is 65. She has done her time. But my reaction. Panic. My thoughts spun. They pushed forward then swung back. I went into a stare. Then tears welled up, went away, and came back as I said, "you can't, you can't do this." As my emotions and ration kicked in I went into what a polite selfless person does and congratulated her. Told her I understood. I began to thank her, because that was in fact my heart, I am thankful. Then I stared some more. She told me I have done an excellent job in Gary's care. She was being sincere, but again, its a natural reaction to smooth it over. She stared at me. Another round of tears came and went. We reminded each other of past treatments, and what a wild ride it has been for Gary. I told her given the severity of Gary's case, that she and her team had done a very impressive job of getting him back and keeping him functioning. I suppose I am so upset with this because as a patient there is a vulnerability of connection. I connect all the bad news that has come with this disease, and the good. Even when I had complaints, there was always praise and gratefulness. I have been mad at her for silly things. But I can't barely remember those. I know it will be alright. I already called and am on the schedule to have another doctor with the same level of experience, whom I respect, take over. She told me I was on the list of patients she was most worried to tell. The emotions this triggers is unbelievable. I do tend to be emotionally dramatic maybe a bit irrational when I hear things I don't care for. Not loud or rude, well maybe but she was right to worry. I'm still trying to entirely connect I'm taking this so hard. I am in the market for a fabulous retirement gift. I know with time I will mend. LOL. Feel like I am going through a break up.
MY BOY
 |
| Calcinosis around tail bone. |
PT
I can't wait till she gets the report on this one. The therapist hit every point I was seeing. His function his there but his strength is not there to support it. He has hip and leg weakness. He straightens his left leg. The therapist said it could be from calcium, "he goes up and down the stairs with a lot of compensation, like leaving his leg straight, pivoting his hip", much like an eighty year old man. I am not sure how many times a week we will be doing physical therapy yet, but the orders will be doing in. Time to get this boy strong or stronger.
SocCoR
Gary is such a sports guy. He loves it. So I signed him up for soccer. Hopefully he will just stand there and look cute so the ball doesn't hit him or anything like that. Doubt it. It will be good for him? Hands over eyes.
Infusion next week. Not looking forward to it.
Tuesday, January 24, 2012
IVIG January Infusion
*Woops forgot to post this.*
Ok. That was terrible.
Ok. That was terrible.
I thought a good night sleep would help me feel better about, but I wake up this morning feeling worse. I feel somewhat selfish saying that. I am not the one who get a needle jammed into my hand (well it was his wrist this time). I am not the one who had drug slowly drip into me making me feel terrible. But I am the mother who has to watch.
Our infusion clinic was recently remodeled. Yesterday I received a call asking if we could go to Bellevue instead. I quickly returned their call and said sure. Then thinking it over I changed my mind. I wanted to keep our appointment because of the reaction Gary had last month. He also had a slight case of the sniffles. I called back and said sorry no, can't move appointments and we need isolation.
I was slightly worried when we arrived at 8am in the morning that our appointment would have been moved but it wasn't. Up at 4:40am, out the house by 6:15am arriving at 8am would be not fun if we didn't have an appointment.
 First order of business was the reaction Gary had last month. The nurse didn't want to start anything without talking to the doctors. I did feel that the benadryl may have just worn off during the last infusion. I explained if we ran the benadryl after the methopred then things may go smoother. She was cautious though and really wanted to talk to the doctors first. When she returned to our room, she explained Dr. E was on her way to talk to me. She explained Gary may not be receiving Ivig and just methopred. I was a little surprised by that. I was not sure how I felt about that. It's a weight issue. Weighing disease activity verses side effects. When the good doctor arrived I explained what had happened last month.
First order of business was the reaction Gary had last month. The nurse didn't want to start anything without talking to the doctors. I did feel that the benadryl may have just worn off during the last infusion. I explained if we ran the benadryl after the methopred then things may go smoother. She was cautious though and really wanted to talk to the doctors first. When she returned to our room, she explained Dr. E was on her way to talk to me. She explained Gary may not be receiving Ivig and just methopred. I was a little surprised by that. I was not sure how I felt about that. It's a weight issue. Weighing disease activity verses side effects. When the good doctor arrived I explained what had happened last month.
I was slightly worried when we arrived at 8am in the morning that our appointment would have been moved but it wasn't. Up at 4:40am, out the house by 6:15am arriving at 8am would be not fun if we didn't have an appointment.
 First order of business was the reaction Gary had last month. The nurse didn't want to start anything without talking to the doctors. I did feel that the benadryl may have just worn off during the last infusion. I explained if we ran the benadryl after the methopred then things may go smoother. She was cautious though and really wanted to talk to the doctors first. When she returned to our room, she explained Dr. E was on her way to talk to me. She explained Gary may not be receiving Ivig and just methopred. I was a little surprised by that. I was not sure how I felt about that. It's a weight issue. Weighing disease activity verses side effects. When the good doctor arrived I explained what had happened last month.
First order of business was the reaction Gary had last month. The nurse didn't want to start anything without talking to the doctors. I did feel that the benadryl may have just worn off during the last infusion. I explained if we ran the benadryl after the methopred then things may go smoother. She was cautious though and really wanted to talk to the doctors first. When she returned to our room, she explained Dr. E was on her way to talk to me. She explained Gary may not be receiving Ivig and just methopred. I was a little surprised by that. I was not sure how I felt about that. It's a weight issue. Weighing disease activity verses side effects. When the good doctor arrived I explained what had happened last month. I was nervous about traffic that morning. The route we take to the hospital now has a toll bridge on it. So, to avoid the toll, we have to take the more traveled way. I left as early as I could. We made excellent time. I know it won't always be like that but I was so relieved. Not to mention the beautiful sunrise. I wished we were going to the airport as we passed the exit.
Dr. E decided to proceed with the IVIG but at 1/2 rate. That meant 10 hours in the infusion center. The IV start was terrible like it always is. We are running out of veins on the tops of his hands. The numbing cream was only put on the tops of his hands. They found a vein in his wrist again. During the iv start he started to try and vomit. He told the nurses through his many tears that he hated his world. None of the full grown adults who have experienced life and its good and bad times, did not like hearing that. I think all of our hearts cracked a little.
Labs came back clear. Meaning no extreme elevated levels. He has one inflammation marker that is up and has been since February of 2011. Our fellow doctor was starting to explain it could be up because of the cold he may have. But she had to eat her words once we saw how it has been bouncing around for a long while now. The doctors came to us again for our clinic visit. This time however, it was a no go. Gary was in no mood.
He actually seemed mentally disturbed. It was crazy. He would not let anyone touch him. He screamed and told them to get away. The doctors would like him to get evaluated by a child life specialist. Help him deal better. We are also going to do another evaluation with physical therapy. He has a little trouble lifting his leg into his pants when dressing. He is also very cautious. Very cautious. He tends to hang on to things for dear life for stability. Its not a weakness per say but there is definite signs of maybe some overall residual muscle damage/weakness.
UPDATE: 01-24-12
Gary is doing better and better. Each day that goes by, you can see the effects of Rituxan kicking in nicely once again. We just thawed out of a snow and ice storm. No power for 2 days. Gary was very inconvenience, lol. He kept running over to things to see if they would work. He asked if we had a little power. He was confused because the water still worked. We had an awesome time sledding. Gary loves it and is able to play in the snow just fine. Walking up the big hill over and over again. He does have a cough that is bothersome but only at night it is really bad. Think he just might have the sniffles.
Dr. E decided to proceed with the IVIG but at 1/2 rate. That meant 10 hours in the infusion center. The IV start was terrible like it always is. We are running out of veins on the tops of his hands. The numbing cream was only put on the tops of his hands. They found a vein in his wrist again. During the iv start he started to try and vomit. He told the nurses through his many tears that he hated his world. None of the full grown adults who have experienced life and its good and bad times, did not like hearing that. I think all of our hearts cracked a little.
Labs came back clear. Meaning no extreme elevated levels. He has one inflammation marker that is up and has been since February of 2011. Our fellow doctor was starting to explain it could be up because of the cold he may have. But she had to eat her words once we saw how it has been bouncing around for a long while now. The doctors came to us again for our clinic visit. This time however, it was a no go. Gary was in no mood.
He actually seemed mentally disturbed. It was crazy. He would not let anyone touch him. He screamed and told them to get away. The doctors would like him to get evaluated by a child life specialist. Help him deal better. We are also going to do another evaluation with physical therapy. He has a little trouble lifting his leg into his pants when dressing. He is also very cautious. Very cautious. He tends to hang on to things for dear life for stability. Its not a weakness per say but there is definite signs of maybe some overall residual muscle damage/weakness.
UPDATE: 01-24-12
Gary is doing better and better. Each day that goes by, you can see the effects of Rituxan kicking in nicely once again. We just thawed out of a snow and ice storm. No power for 2 days. Gary was very inconvenience, lol. He kept running over to things to see if they would work. He asked if we had a little power. He was confused because the water still worked. We had an awesome time sledding. Gary loves it and is able to play in the snow just fine. Walking up the big hill over and over again. He does have a cough that is bothersome but only at night it is really bad. Think he just might have the sniffles.
 |
| A very special gift from our fellow JDM friend Sue and Kristen. Gary's new favorite. |
Subscribe to:
Posts (Atom)